Azelaic Acid for Melasma During Pregnancy: Dermatologist-Recommended Guide
You saw the movies. You read the books. You expected the “pregnancy glow.” What you didn’t expect was that the second or third trimester would bring with it an unwelcome shadow: dark, splotchy patches spreading across your forehead, cheeks, or upper lip.
If this sounds familiar, you’ve likely met the “mask of pregnancy,” also known as melasma during pregnancy.
This common form of hyperpigmentation is entirely harmless to your baby, yet it can be a significant source of emotional distress and self-consciousness. Suddenly, you’re faced with a dilemma: you desperately want to treat the discoloration, but you are rightly terrified of using anything that could potentially harm your developing child.
You need a solution that is both effective against stubborn dark patches and unequivocally pregnancy-safe.
The good news is that such an ingredient exists, and dermatologists back it as the first-line defense for expectant mothers: azelaic acid.
Want to understand how other brightening ingredients like vitamin C, niacinamide, and alpha arbutin work at a cellular level? Our comprehensive guide breaks down the best skincare ingredients for hyperpigmentation and how they target dark spots.
This article is your comprehensive guide to reclaiming your complexion. We’ll dive deep into the safety profile of azelaic acid, explain how it works to fight the pregnancy mask, provide step-by-step instructions for using it while pregnant, and set realistic expectations for your journey to clearer, more even skin.
What is pregnancy-related melasma?
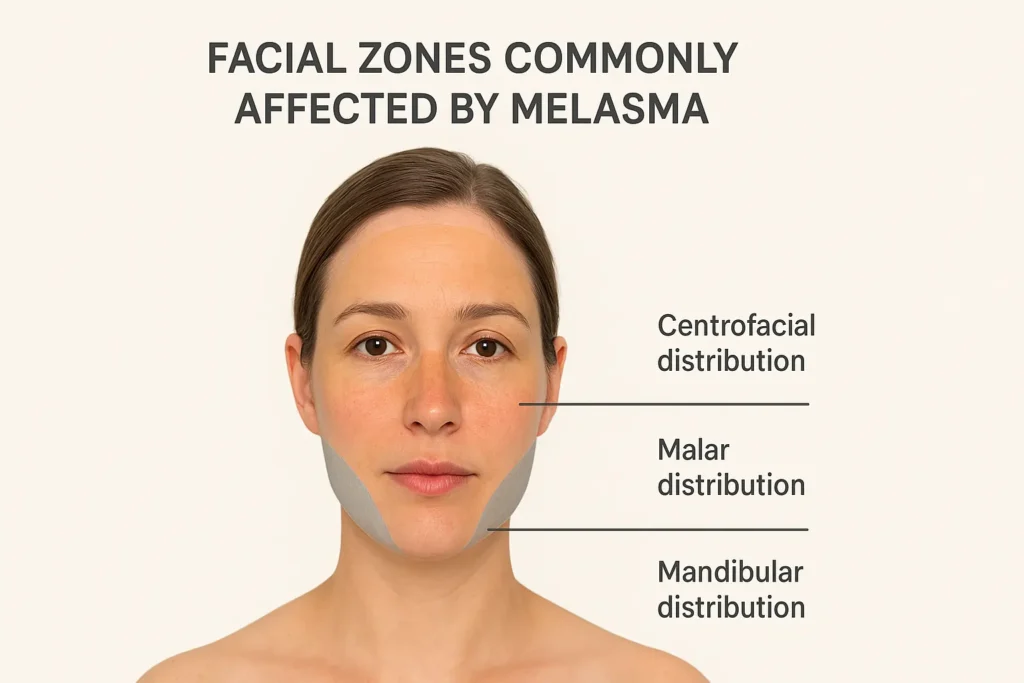
Pregnancy-related melasma is a common form of hormonal hyperpigmentation that appears as brown or gray-brown patches on the face during pregnancy. Triggered by hormonal shifts and sun exposure, it most often affects the cheeks, forehead, upper lip, and nose. It’s harmless—but emotionally and cosmetically challenging for many women.
Over nearly two decades of work in medicine and cosmetic science, I’ve seen how unexpectedly distressing this can feel. Often called the “mask of pregnancy,” melasma affects an estimated 15 to 50% of pregnant women according to clinical reviews.
Understanding the “Mask of Pregnancy”
Melasma develops when melanocytes (pigment-producing cells) become overstimulated and produce excess melanin. That pigment migrates into surrounding skin cells, forming visible patches ranging from light tan to deep brown or gray, depending on depth.
Common melasma patterns:
-
Centrofacial: Forehead, cheeks, nose, upper lip
-
Malar: Cheeks and nose
-
Mandibular: Jawline and chin
Dermatology research shows that melasma can significantly affect quality of life, increasing self-consciousness during pregnancy. The condition is cosmetic—not dangerous—but the emotional impact is real.
What Causes Pregnancy Melasma?
Pregnancy melasma stems from a perfect storm of hormones and light exposure. Rising estrogen, progesterone, and melanocyte-stimulating hormone (MSH) signal melanocytes to overproduce pigment—especially during the second and third trimesters.
Key contributing factors include:
-
Hormonal fluctuations (primary trigger)
-
UV and visible light exposure, which intensifies pigmentation
To understand how the right sunscreen can protect melasma-prone skin during pregnancy, read our complete, dermatologist-backed guide here:
-
Genetic predisposition (family history increases risk)
The reassuring news? Pregnancy-related melasma is harmless to both parent and baby—and many cases fade postpartum with the proper care, patience, and sun protection.
Why Azelaic Acid Is the Safest Treatment for Melasma During Pregnancy
Yes—azelaic acid is considered safe during pregnancy and is widely recommended for melasma by dermatologists. It reduces excess pigment and inflammation with minimal skin absorption, meaning it does not enter the bloodstream in significant amounts. Decades of clinical use and guideline support make it a first-line, pregnancy-safe option.
Drawing on my 18+ years in medicine and cosmetic science, azelaic acid consistently stands out as the rare ingredient that balances efficacy, safety, and tolerability during pregnancy—when treatment options are otherwise limited.
What’s The Science Behind Azelaic Acid?
Azelaic acid is a naturally occurring dicarboxylic acid derived from grains like barley, wheat, and rye. What makes it special for pregnancy melasma treatment is its targeted mechanism: it inhibits tyrosinase, the enzyme responsible for melanin production, while simultaneously reducing the transfer of pigment to your skin’s surface.
According to research published in the International Journal of Dermatology, azelaic acid also provides antioxidant protection against free radicals that can worsen hyperpigmentation. It’s genuinely multi-functional—treating melasma, pregnancy acne, and redness all at once.

Pregnancy Safety Profile Of Azelaic Acid
Azelaic acid is classified as FDA Pregnancy Category B, meaning animal studies show no fetal risk. Its minimal systemic absorption is why dermatologists consider it pregnancy-safe. Dr. Joshua Zeichner, MD, notes it “remains on the skin rather than entering circulation”. ACOG also recognizes topical azelaic acid as safe during pregnancy.

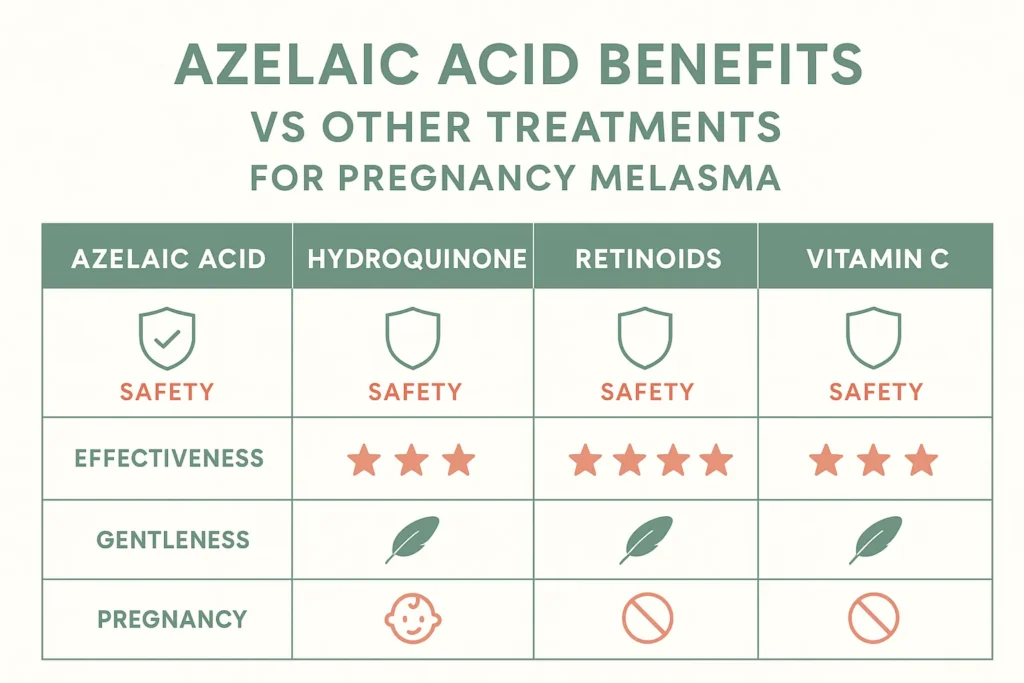
Let’s contrast this with what you absolutely should avoid:
- ❌ Hydroquinone: Insufficient safety data; up to 35% systemic absorption makes it risky
- ❌ Retinoids/Retinol: Known teratogen (can cause birth defects)
- ❌ High-dose Salicylic Acid: Oral forms linked to birth defects; topical high concentrations avoided
- ✅ Azelaic Acid: FDA Category B, minimal absorption, extensively used
- ✅ Vitamin C: Safe antioxidant that complements azelaic acid
- ✅ Niacinamide: Gentle, practical, no pregnancy concerns
The American College of Obstetricians and Gynecologists considers topical azelaic acid safe for use throughout pregnancy when discussing pregnancy-safe acne treatments, including melasma treatment.
What Dermatologists Say
Board-certified dermatologists consistently recommend azelaic acid for melasma during pregnancy. It’s no surprise that board-certified dermatologist Dr. Hadley King, MD, calls azelaic acid the ‘cornerstone of pregnancy-safe melasma treatment.’
Beyond its proven safety profile, its unique multitasking benefits allow you to treat both pigmentation and hormonal breakouts simultaneously. That said, because every pregnancy is exceptional, I always advise discussing any new treatment with your OB-GYN to ensure it aligns with your personal medical history.
How Azelaic Acid Works to Treat Melasma?
Azelaic acid treats melasma by gently regulating pigment production and distribution in the skin. It inhibits excess melanin production, reduces pigment transfer to surface skin cells, and protects against inflammation and UV-related damage. This gradual, targeted action makes azelaic acid effective yet safe, including during pregnancy.
Understanding Melasma in Simple Terms
Melasma develops through a step-by-step pigmentation process:
-
Melanocytes (pigment cells) produce melanin
-
Melanin is transferred to surrounding skin cells
-
Excess buildup appears as dark patches on the face
Hormonal changes and UV exposure overstimulate this process—especially during pregnancy.
Azelaic acid works by interrupting multiple steps of this pathway without shutting pigment production down completely.
Three Ways Azelaic Acid Fights Melasma
1. Inhibits Melanin Production
Azelaic acid acts as a tyrosinase inhibitor, safe in pregnancy, targeting the enzyme required for melanin synthesis.
-
Slows the overproduction of pigment
-
Helps prevent new dark patches from forming
-
Supports a more balanced, even skin tone
This is why it’s often described as a melanin inhibitor in pregnancy rather than a bleaching agent.
2. Reduces Existing Pigmentation
Azelaic acid interferes with melanin transfer from melanocytes to surface skin cells.
-
Limits pigment accumulation in the epidermis
-
Gradually fades existing melasma patches
-
Improves clarity without causing rebound pigmentation
Results appear steadily over weeks, not days.
3. Provides Antioxidant Protection
UV exposure generates free radicals that worsen pigmentation.
Azelaic acid:
-
Neutralizes oxidative stress
-
Reduces UV-triggered pigment signaling
-
Helps prevent future melasma darkening when paired with sunscreen
Additional Skin Benefits That Support Melasma Control
-
Gentle exfoliation helps shed pigmented surface cells
-
Anti-inflammatory action calms hormonally sensitive skin
-
Suitable for long-term, daily use
Importantly, azelaic acid works gradually, reducing the risk of irritation and supporting a natural-looking improvement.
Benefits Of Using Azelaic Acid For Melasma During Pregnancy
Azelaic acid is one of the safest and most effective treatments for pregnancy melasma. It gently lightens dark spots, prevents new pigmentation, calms inflammation, and improves acne and redness—without significant systemic absorption. Backed by decades of clinical use, it delivers gradual, natural-looking results suitable for all trimesters.
After nearly two decades in medicine and cosmetic formulation science, it’s the ingredient I trust most when safety and results must coexist.
Primary Benefits
1. Lightens Dark Patches Safely
Azelaic acid reduces melasma by inhibiting tyrosinase, the key enzyme in melanin production. Unlike bleaching agents, it normalizes pigment activity rather than stripping skin color.
Patience is your best friend when treating the pregnancy mask. Clinical reviews published in the Journal of Drugs in Dermatology confirm that while the healing begins immediately, visible improvement typically peaks within 8–12 weeks. This timeline allows for even-toned, natural-looking results that don’t look ‘bleached’ or artificial.
2. Prevents New Pigmentation
One of the most significant—yet often overlooked—benefits of azelaic acid for pregnancy-related melasma is its preventive effect. During the hormonal peaks of your second and third trimesters, your body is essentially ‘ordering’ your skin to produce more pigment.
3. Gentle Yet Effective For Sensitive Pregnancy Skin
Pregnancy often increases skin reactivity, making harsh treatments like retinoids risky. Dr. Marisa Garshick notes that azelaic acid’s gentle approach is “ideal for the increased sensitivity many women experience during pregnancy,” allowing it to treat melasma safely without irritation. Always consult your OB-GYN before starting new routines.
4. Multi-Tasking Formula
Azelaic acid treats melasma, pregnancy acne, redness, and texture simultaneously. Its antibacterial and anti-inflammatory actions reduce breakouts while calming hormonally sensitive skin—simplifying routines when minimalism matters most.

Beyond visible results, azelaic acid offers “Category B” peace of mind—it’s safe for the baby throughout all trimesters and breastfeeding. Unlike other acids, it won’t cause photosensitivity. The American Academy of Dermatology confirms that its minimal absorption makes it safe for continuous use, allowing you to maintain progress from pregnancy through the postpartum period.
How To Use Azelaic Acid For Melasma During Pregnancy
To use azelaic acid safely during pregnancy, select the dermatologist-recommended concentration, apply it to completely dry skin, and use it consistently. Start slowly, prioritize sun protection, and avoid mixing it with unsafe actives. When used correctly, azelaic acid delivers gradual improvement in melasma with minimal irritation and strong evidence of pregnancy safety.
After 18+ years in medicine and cosmetic formulation, I’ve learned that application technique matters as much as the ingredient itself—especially during pregnancy.
Choosing The Right Azelaic Acid Product
Start with 10% azelaic acid if you’re new to azelaic acid or have sensitive pregnancy skin. For established melasma, 15–20% formulations (often prescription) are more effective.
-
Creams: best for dry skin
-
Gels: ideal for acne-prone skin
-
Serums: lightweight, fast-absorbing
According to research in Clinical, Cosmetic and Investigational Dermatology, the vehicle (cream vs. gel) can affect both efficacy and tolerability, so choose based on your skin type.
When reading labels, look for pregnancy-safe certifications if available, and absolutely avoid products that combine azelaic acid with retinoids or hydroquinone—these ingredients aren’t safe during pregnancy.
Fragrance-free formulas are strongly preferred since pregnancy often increases scent sensitivity and fragrance can irritate melasma-prone skin.
Dr. Whitney Bowe, a board-certified dermatologist and clinical assistant professor at Mount Sinai, emphasizes that “simple, fragrance-free formulations minimize the risk of irritation during pregnancy when skin barrier function may be compromised”.

Step-By-Step Application Guide
Consistency and proper layering are essential when using azelaic acid during pregnancy.
For a step-by-step routine that shows how azelaic acid fits into a complete pigmentation-focused regimen, see our full guide: Skincare Routine for Hyperpigmentation
Morning Routine:
In the morning, cleanse with a gentle, non-foaming cleanser and allow skin to fully dry. If tolerated, apply vitamin C, then finish with a broad-spectrum SPF 50+ sunscreen, which is critical for preventing melasma from worsening.
For a deeper explanation of how daily sun protection supports pigment control and skin aging, see our complete guide to sun protection and anti-aging.
Evening Routine:
In the evening, cleanse thoroughly to remove sunscreen and impurities. Wait until skin is completely dry before applying a pea-sized amount of azelaic acid to affected areas only. Allow it to absorb for 10–15 minutes, then follow with a pregnancy-safe moisturizer. This method minimizes irritation while maximizing effectiveness.

How Often To Use Azelaic Acid
From both clinical practice and research, I’ve learned that consistency matters more than strength, especially during pregnancy. Start with once-daily evening use for the first week. If well tolerated, increase to twice daily.
Patch Test Instructions
I always recommend patch testing—even if you’ve used azelaic acid before pregnancy. Hormonal shifts can change skin sensitivity overnight. Apply a rice-grain amount to your inner wrist or behind the ear, wait 24 hours, and check for redness, itching, burning, or swelling.
The American Contact Dermatitis Society advises patch testing during pregnancy due to immune changes. If you react, don’t apply it to your face—see a dermatologist instead.
Damp or dehydrated skin increases absorption too quickly and may trigger tingling or irritation—especially during pregnancy, when the skin barrier is naturally more sensitive.
What’s The Best Pregnancy-Safe Skincare Routine For Melasma?
The best pregnancy-safe skincare routine for melasma combines azelaic acid, strict mineral sun protection, antioxidants, and barrier support. Used consistently, this layered approach helps fade existing pigmentation, prevent new dark patches, and protect hormonally sensitive skin—without ingredients known to pose pregnancy risks.
Below is the dermatologist-aligned, evidence-based routine I recommend.
Your Complete Morning Routine
Step 1: Gentle Cleanser
Start with a fragrance-free, sulfate-free cleanser that won’t strip your already-sensitive pregnancy skin. Cream cleansers work beautifully for dry skin, while micellar water offers a no-rinse option for mornings when you’re battling nausea.
Step 2: Vitamin C Serum (10-20% L-Ascorbic Acid)
This step provides antioxidant protection against UV-induced pigmentation, brightens existing dark spots, and prevents new melasma patches from forming. Apply to completely dry skin and wait 1-2 minutes for absorption. Research published in the Journal of the American Academy of Dermatology demonstrates that combining topical vitamin C with sunscreen provides superior photoprotection against UV damage compared to sunscreen alone.
Pregnancy-safe vitamin C serums include SkinCeuticals C E Ferulic (gold standard for stability), Timeless 20% Vitamin C + E Ferulic Acid Serum (excellent budget option), or Mad Hippie Vitamin C Serum (affordable and practical).
Step 3: [Optional] Azelaic Acid
Once you’ve established tolerance to azelaic acid in your evening routine, you can add it to your morning routine as well. Apply after vitamin C and wait 10 minutes before sunscreen to ensure proper absorption.
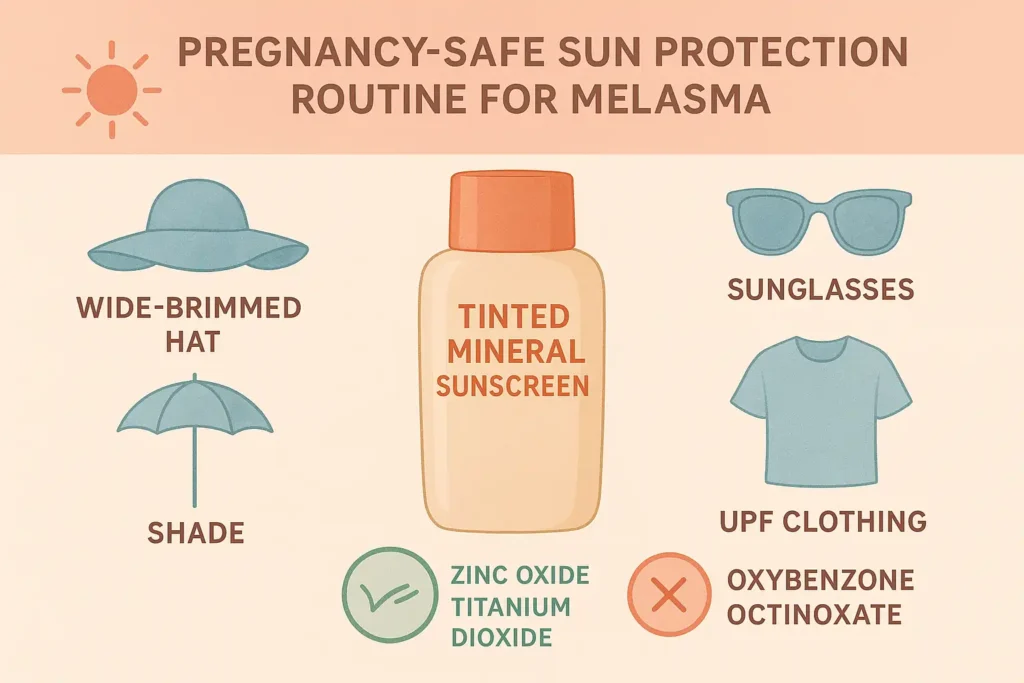
Step 4: Mineral Sunscreen SPF 50+
This is the most critical step for melasma management—non-negotiable, every single day. Choose tinted formulas containing iron oxides to block visible light, which can trigger melasma as much as UV. Physical blockers only: zinc oxide and titanium dioxide. The American Academy of Dermatology emphasizes that “sunscreen is the foundation of all melasma treatment”. Reapply every two hours when outdoors.
Your Complete Evening Routine
Step 1: Double Cleanse (If Wearing Makeup/Sunscreen)
Start with an oil cleanser or micellar water to break down sunscreen and makeup, then follow with a gentle face wash to remove remaining residue. This ensures clean skin that’s ready to absorb treatment products.
Step 2: [Optional] Niacinamide Serum
Niacinamide complements azelaic acid beautifully by reducing pigment transfer through a different mechanism. It also strengthens your skin barrier during pregnancy, when hormonal changes may compromise it. Apply before azelaic acid and wait about five minutes.
Step 3: Azelaic Acid
Apply to bone-dry skin—this is crucial for minimizing irritation. Wait 10-15 minutes before moving to the next step to allow proper penetration.
Step 4: Hydrating Moisturizer
Look for ceramides and hyaluronic acid to repair and hydrate. Fragrance-free formulas are essential during pregnancy when scent sensitivity increases and fragrance can irritate melasma-prone skin.
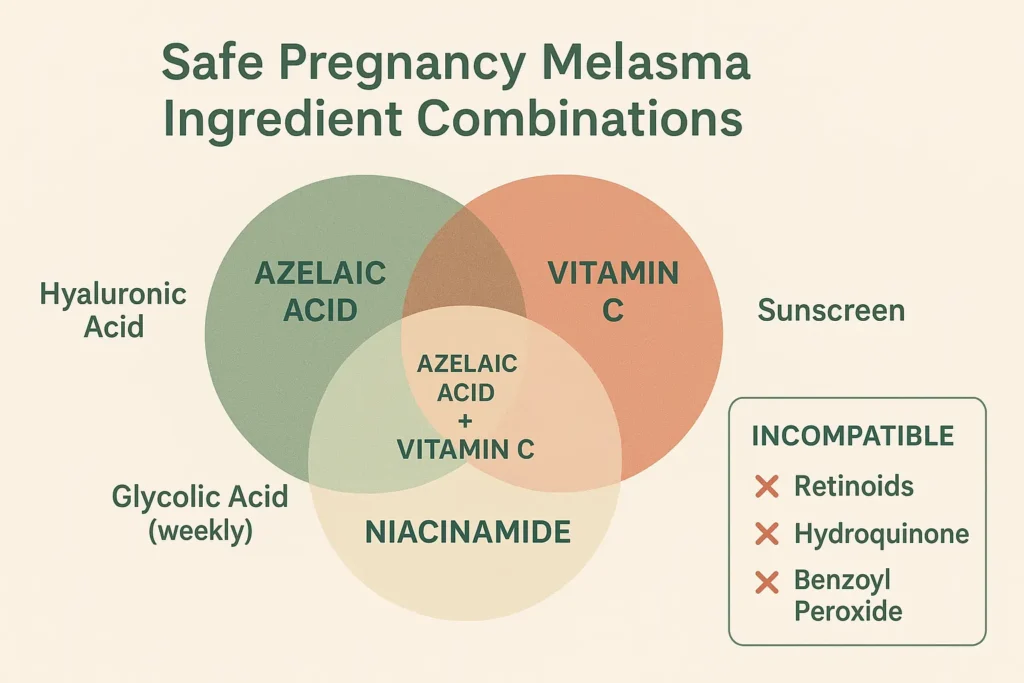
Weekly Add-Ons (Optional)
-
Low-Strength Glycolic Acid (10–25%, 1–2× weekly)
Improves texture and penetration. Never use on the same night as azelaic acid. -
Hydrating Masks
Calm inflammation and support barrier recovery.
What NOT To Mix With Azelaic Acid
- ❌ Retinoids (pregnancy-unsafe anyway)
- ❌ Benzoyl peroxide (may cause excessive dryness when combined)
- ❌ Multiple strong exfoliants on the same day (compromises skin barrier)
- ✅ Vitamin C – safe and synergistic
- ✅ Niacinamide – safe and complementary
- ✅ Hyaluronic acid – safe hydration booster
- ✅ Sunscreen – essential daily combination
Is Sun Protection The Non-Negotiable Partner To Azelaic Acid?
After nearly two decades in skincare science, I can say this clearly: azelaic acid cannot outwork sun exposure. During pregnancy, hormonal shifts heighten melanin activity, making UV and visible light the primary drivers of melasma relapse. Sunscreen isn’t an add-on—it’s the structural support that allows azelaic acid to work predictably, safely, and consistently.
Why Sunscreen Is Essential For Melasma
UV and visible light activate melanocytes, rapidly increasing melanin production. In pregnancy, this response is amplified by estrogen and progesterone. Research in JAMA Dermatology shows that even short UV exposure can reverse months of melasma improvement, making daily sun protection essential—not optional.
ACOG also confirms increased pregnancy-related photosensitivity:
Best Sunscreen Practices During Pregnancy
Your best sunscreen for melasma during pregnancy should meet several non-negotiable criteria—first, a minimum SPF of 50+ with broad-spectrum protection covering both UVA and UVB rays. Don’t settle for SPF 30—studies show that real-world application typically delivers only 50-75% of the labeled SPF, so starting higher gives you a safety buffer.
Mineral or physical sunscreens containing zinc oxide and titanium dioxide are strongly preferred during pregnancy. Unlike chemical sunscreens that absorb into your skin and potentially your bloodstream, physical blockers sit on your skin’s surface and reflect UV rays away. The Environmental Working Group’s research confirms that mineral sunscreens pose zero known risks to pregnant women or developing babies.
Expert Guide: To learn how proper sun protection supports melasma prevention and long-term skin health, read our complete, dermatologist-backed guide here.
Tinted Formulas are Game-Changers for Melasma
They contain iron oxides that block visible light—the part of the light spectrum that research increasingly shows triggers melasma just as much as UV radiation. Dr. Iltefat Hamzavi, Senior Staff Physician at Henry Ford Hospital, has published extensive research demonstrating that visible light protection is “essential for comprehensive melasma management, particularly in skin of color”.
Reapply every two hours when outdoors—set a phone reminder if needed. And sunscreen is just the beginning of your protection strategy.
Learn More: To learn why zinc oxide–based formulas are especially effective for pigment-prone and sensitive skin, read our in-depth guide here.
Additional protection measures:
- Wide-brimmed hats (at least 3-inch brim all around)
- Seek shade between 10am-4pm when UV radiation peaks
- UV-protective sunglasses (wrap-around style blocks more light)
- UPF 50+ rated clothing for extended outdoor activities
What are the Top Sunscreen Ingredients For Pregnancy?
The safest sunscreen ingredients during pregnancy are mineral filters, such as zinc oxide and titanium dioxide. They provide broad-spectrum UVA/UVB protection, sit on the skin’s surface, and show minimal absorption. Avoid chemical filters like oxybenzone and octinoxate, which absorb systemically and raise hormonal safety concerns during pregnancy.
☀️ Critical Reminder: One minute of unprotected sun exposure can undo one year of melasma treatment.
Make SPF your best friend—apply it as your skin depends on it, because when it comes to melasma, it absolutely does.
What To Expect: Results Timeline For Pregnancy Melasma
Azelaic acid gradually improves pregnancy-related melasma, not overnight. Expect skin adjustment in the first two weeks, subtle brightening by weeks 3–4, visible fading by weeks 6–8, and optimal improvement by weeks 10–12. Complete clearance often occurs postpartum as hormones normalize, especially with consistent sun protection.
After spending years in cosmetic science and patient care, I have found that managing expectations is the single most significant factor in treatment success.
Week-By-Week Progress Guide
Weeks 1-2: Adjustment Phase
Your skin is acclimating. Mild tingling, warmth, or dryness can occur and usually settles quickly. No visible pigment change yet—this is normal.
What to do: Focus on tolerance, reduce frequency if needed, and use SPF 50+ daily. Early consistency matters more than speed.
Weeks 3-4: Early Changes
Skin texture improves first—smoother, brighter, more even-feeling skin. Pigment changes are subtle but begin at a cellular level. Research confirms melanin regulation precedes visible fading.
What to do: Maintain daily use; increase to twice daily only if well tolerated.
Weeks 6-8: Noticeable Improvement
Melasma patches visibly lighten, and overall tone evens out. New pigmentation is better controlled. Dermatologist Dr Zoe Draelos notes that this is when many patients first feel encouraged by results.
What to do: Stay consistent—don’t increase strength or frequency.
Weeks 10-12: Optimal Results During Pregnancy
At the 10-12 week milestone, you’ll notice significant fading of dark patches—the difference from your starting point should be substantial. Your melasma is stabilized, meaning it’s not worsening despite ongoing hormonal surges—your confidence and comfort in your skin are improving, which matters just as much as the physical changes.
For a look at what these stages actually look like on real skin, please browse our gallery of Azelaic Acid Before & After: 12 Real Results.
Melasma often doesn’t fully clear during pregnancy, and that’s normal. Elevated hormones continue to stimulate pigment. The goal is prevention and gradual improvement. Research shows melasma responds best postpartum, when hormones stabilize, and treatment becomes more effective.
Postpartum: 3-12 Months After Delivery
As hormones normalize, fading often accelerates. Many women see near-complete resolution with continued azelaic acid, which is considered compatible with breastfeeding. Stronger treatments can be regarded as later if needed.

Managing Your Expectations
Melasma is a long-term condition. Dr. Susan Taylor emphasizes that success means stabilization first, fading second—not overnight clearance.
Key takeaway:
If melasma isn’t worsening during pregnancy, your routine is working. Consistency + sun protection = results.
Factors That Affect Results
Faster results typically occur with:
- Early treatment initiation (starting in the second trimester vs. the third)
- Consistent daily sunscreen use without exception
- Lighter skin tones (though melasma is less common)
- Epidermal melasma (pigment in upper skin layers responds faster)
Slower results typically occur with:
- Late treatment start (beginning in the third trimester)
- Poor or inconsistent sun protection
- Deeper dermal melasma (pigment in lower skin layers)
- Darker skin tones (more melanin means more to regulate)
- High sun exposure lifestyle
Individual variation factors:
- Genetic predisposition to pigmentation disorders
- Pregnancy hormone levels (vary widely between women)
- Skin sensitivity and barrier function
- Stress levels (emerging research links cortisol to pigmentation)
🌟 Patience Pays Off: Preventing melasma from worsening during pregnancy is just as crucial as lightening it.
With consistent azelaic acid use and daily sun protection, you’re on the right path—many of the best results appear postpartum as hormones settle.
What Are The Possible Side Effects Of Azelaic Acid And How Can You Minimize Them?
I consistently reassure expecting parents that azelaic acid is considered pregnancy-safe, but hormonally sensitive skin still requires a cautious, respectful approach. Mild side effects may occur as skin adjusts, yet they’re typically temporary, predictable, and easily minimized with proper application, gradual use, and realistic expectations.
Common Side Effects (Usually Mild)
1. Tingling Or Mild Burning
A brief tingling or warmth within the first 5–10 minutes is the most common early reaction. It reflects skin adjustment, not damage, and typically fades within 1–2 weeks. Clinical reviews in the Journal of Drugs in Dermatology confirm this response is benign and self-limiting.
2. Dryness Or Flaking
Azelaic acid mildly normalizes cell turnover, which can cause early dryness. Applying a fragrance-free moisturizer 10–15 minutes later, and temporarily reducing the frequency, usually resolves this. Always apply to completely dry skin, as damp skin increases absorption and the risk of irritation.
3. Temporary Redness
Mild redness or flushing that fades within 20–30 minutes can occur, particularly in pregnancy-sensitive skin. Using a pea-sized amount helps. Board-certified dermatologist Dr. Sejal Shah notes this reaction typically resolves as tolerance builds.
When To Stop Using Azelaic Acid
Stop use and consult your dermatologist or OB-GYN if you experience:
-
Persistent burning or pain
-
Blistering or significant peeling
-
Hives, swelling, or allergy symptoms
-
Irritation lasting beyond two weeks
The American Academy of Dermatology notes these reactions are rare but should be addressed promptly during pregnancy.

Minimizing Irritation Tips
-
Start with 10% azelaic acid, once daily at night
-
Apply only to bone-dry skin
-
Use gentle, fragrance-free cleansers and moisturizers
-
Avoid broken or inflamed skin
-
Increase frequency slowly as tolerance develops
Key Takeaway: When used thoughtfully, azelaic acid side effects during pregnancy are typically mild, manageable, and temporary—making it one of the most reliable, evidence-supported options for melasma and hormonally sensitive skin.
Combining Azelaic Acid With Other Pregnancy-Safe Treatments
Azelaic acid is most effective for pregnancy-related melasma when paired with complementary, pregnancy-safe ingredients that target pigmentation through different pathways. Strategic combinations—used at the right time and frequency—can improve fading, prevent new patches, and protect the skin barrier without increasing irritation. Thoughtful layering matters more than adding many actives.
After nearly two decades formulating protocols, I’ve learned that synergy beats strength during pregnancy.
Best Companion Ingredients For Azelaic Acid
1. Vitamin C (L-Ascorbic Acid 10-20%)
Vitamin C provides antioxidant protection, limits UV-triggered melanin, and enhances brightening. Use in the morning before sunscreen; pair azelaic acid at night or both once tolerated. Combination therapy shows superior outcomes versus monotherapy in pigment disorders:
Pregnancy-safe options include SkinCeuticals C E Ferulic and Timeless 20% Vitamin C.
2. Niacinamide (Vitamin B3, 5-10%)
Niacinamide reduces melanin transfer and strengthens the skin barrier—key for hormonally sensitive pregnancy skin. Apply before azelaic acid or use AM/PM separately. Dr. Leslie Baumann, MD, highlights the excellent tolerability and versatility of pregnancy skincare.
This combination is safe and gentle for pregnancy, particularly suited for sensitive skin, barrier repair needs, and reducing inflammation that can worsen melasma.
If you’re unsure whether vitamin C or niacinamide is better for your skin type and pigmentation concerns, we break down the science in our comparison guide: Vitamin C vs Niacinamide: Which Is Best for Skin?
3. Tranexamic Acid (2-5%)
Tranexamic Acid (2–5%):
Tranexamic acid targets melasma via a plasmin-mediated pathway, complementing azelaic acid’s tyrosinase inhibition. Introduce slowly and consult your OB-GYN or dermatologist due to limited pregnancy-specific topical data. Best reserved for stubborn melasma unresponsive to first-line options.
4. Glycolic Acid (10-25% For At-Home Peels)
Low-strength glycolic acid gently exfoliates and improves penetration. Use 1–2 times per week; do not use on the same night as azelaic acid. ACOG considers low concentrations acceptable during pregnancy when used appropriately.
5. Hyaluronic Acid
A hydration essential that supports tolerance and barrier health. It’s pregnancy-safe, non-interfering, and can be layered before or after azelaic acid to reduce dryness and improve comfort.
Sample Combination Routines
Routine 1: Maximum Brightening (Non-Sensitive Skin)
- AM: Cleanser → Vitamin C → Azelaic Acid → SPF 50+
- PM: Cleanser → Niacinamide → Azelaic Acid → Moisturizer
- Weekly: Glycolic peel (replaces PM routine 1x/week)
Routine 2: Gentle Approach (Sensitive/Reactive Skin)
- AM: Cleanser → Vitamin C → SPF 50+
- PM: Cleanser → Azelaic Acid → Moisturizer
- Weekly: Skip actives 1-2 nights for recovery
Routine 3: Budget-Friendly Basics
- AM: Cleanser → Azelaic Acid → SPF 50+
- PM: Cleanser → Azelaic Acid → Moisturizer
What NOT To Combine
- ❌ Retinoids (pregnancy-unsafe—don’t use at all)
- ❌ Hydroquinone (pregnancy-unsafe—avoid completely)
- ❌ Multiple strong acids same day (over-exfoliation compromises barrier)
- ❌ Benzoyl peroxide + azelaic acid (excessive dryness risk)
- ❌ Vitamin C + glycolic acid simultaneously (too irritating for most skin)
What Professional Treatments Are Safe for Melasma During Pregnancy?
Professional melasma treatments during pregnancy must be conservative. Hormonal shifts make pigment unstable, so most in-office care focuses on maintenance—not correction. A few dermatologist-supervised options are considered safe, but aggressive procedures are avoided.
In most cases, meaningful pigment correction is safest and more effective when deferred until the postpartum period, after hormones stabilize.
Safe Professional Treatments While Pregnant
Low-Concentration Chemical Peels
Superficial peels may be used selectively for chemical peels, pregnancy, and melasma under expert care.
-
Safe options: Glycolic acid (10–25%), lactic acid (20–30%)
-
Benefits: Gentle exfoliation of pigmented cells, improved topical absorption
-
Frequency: Every 2–4 weeks
-
Important: Only with a dermatologist experienced in pregnancy skin
-
Avoid: Salicylic acid, TCA, Cosmelan/Dermamelan peels
The American College of Obstetricians and Gynecologists notes glycolic and lactic acids are generally acceptable when medically supervised:
LED Light Therapy
LED therapy is a non-invasive option sometimes discussed in clinics.
-
Safety: No UV, no heat—generally considered safe
-
Effectiveness: Minimal for melasma itself
-
Better suited for: Pregnancy, acne, and inflammation
Dr. Shari Marchbein, MD (Board-Certified Dermatologist), notes:
“LED therapy won’t worsen melasma, but patients shouldn’t expect pigment clearance.”
Dermaplaning
A physical exfoliation technique is performed with a sterile blade.
-
Safety: Safe when done professionally
-
Benefit: Enhances product penetration
-
Caution: Can irritate hormonally sensitive, melasma-prone skin
Treatments To Avoid Until After Pregnancy
Laser Treatments (IPL, Pico, Q-switched)
Despite popularity, laser treatment for melasma during pregnancy is discouraged.
-
Hormones make outcomes unpredictable
-
High rebound hyperpigmentation risk
-
Safest timing: 3–6 months postpartum
Microneedling
-
Increased infection risk during pregnancy
-
Hormonal healing response is unpredictable
High-Strength Chemical Peels
-
TCA, Jessner’s, phenol peels
-
Too aggressive and inflammatory during pregnancy
The American Academy of Dermatology advises deferring aggressive procedures.
Postpartum Treatment Options
After delivery, treatment options expand significantly.
-
Can begin 3–6 months postpartum (after breastfeeding, if applicable)
-
Options include:
-
Pico or Q-switched lasers
-
Prescription hydroquinone
-
Stronger chemical peels
-
Importantly, many women experience natural improvement of melasma postpartum, reducing the need for aggressive intervention.
What Lifestyle Tips Help Manage Melasma During Pregnancy?
Lifestyle habits play a significant role in managing pregnancy-related melasma alongside topical treatments such as azelaic acid. Consistent sun protection, stress reduction, balanced nutrition, adequate sleep, and gentle skincare help calm inflammation and limit pigment triggers. In practice, combining these habits with pregnancy-safe actives leads to steadier, more sustainable improvement.
Diet And Nutrition
Diet and Nutrition: No food “cures” melasma, but antioxidant-rich nutrition helps skin respond better to treatment.
Focus on:
-
Berries, citrus, and leafy greens (reduce oxidative stress)
-
Omega-3 sources like salmon and walnuts (support barrier health)
-
Adequate hydration (8–10 glasses daily)
Vitamin D should come from diet or supplements—not sun exposure. The Journal of the American Academy of Dermatology notes that vitamin D deficiency may influence inflammatory skin conditions.
Stay hydrated with 8-10 glasses of water daily—adequate hydration supports skin barrier function, which is crucial when using active treatments such as azelaic acid.
Stress Management
Stress Management: Psychological stress elevates cortisol levels, which can exacerbate pigmentation through inflammatory pathways. Research in Experimental Dermatology links stress with increased melasma severity.
Helpful strategies:
-
Prenatal yoga or gentle stretching
-
Mindfulness or guided breathing
-
Consistent sleep (7–9 hours)
-
Sun-protected outdoor walks
Dr. Amy Wechsler, MD (dermatologist & psychiatrist), emphasizes the mind-skin link in pigment disorders.
Habits To Avoid
Habits To Avoid:
-
Picking, waxing, or scrubbing pigmented areas
-
Over-exfoliation or heat exposure (saunas, hot yoga)
-
Skipping sunscreen—even once
UV and heat directly stimulate melanocytes and can undo weeks of progress.
Makeup Tips For Camouflage
Makeup Tips For Camouflage: Peach or orange correctors neutralize brown patches. Apply mineral SPF first, then makeup. Camouflage supports confidence—but treatment consistency creates lasting change.
Emotional Well-Being Matters
Emotional Well-Being Matters: Melasma affects up to 70% of pregnant women. Research confirms its quality-of-life impact. Your feelings are valid—and this phase is temporary.
Actionable Takeaway: Gentle routines, daily sun protection, stress reduction, and patience work together. You’re supporting both your skin and your growing baby—and that matters most.

When To See A Dermatologist About Pregnancy Melasma
You should see a dermatologist for pregnancy melasma if dark patches worsen rapidly, don’t improve after 8–12 weeks of consistent azelaic acid and sunscreen use, cause significant emotional distress, or appear atypical. Early professional guidance ensures accurate diagnosis, pregnancy-safe treatment choices, and realistic expectations during and after pregnancy.
What I’ve learned is that timely specialist care often saves months of frustration.
You Should Consult A Dermatologist If:
-
Pigmentation appears suddenly or worsens quickly
-
Over-the-counter azelaic acid fails after 8–12 weeks
-
Irritation persists despite reduced frequency
-
Melasma affects mental well-being and confidence
-
Diagnosis is unclear (melasma vs PIH or other conditions)
The American Academy of Dermatology notes that several pigment disorders can mimic melasma and require different management.
What To Expect At Your Appointment
Your dermatologist will examine your skin visually and may use a Wood’s lamp to assess pigment depth. Expect questions about pregnancy timing, sun exposure, family history, and current products.
Dr. Adam Friedman, MD, emphasizes thorough history-taking due to limitations in the treatment of pregnancy.
Treatment plans often include prescription azelaic acid (15–20%), safe combination routines, and tailored sun-protection strategies.
Follow-up appointments are typically scheduled every 8-12 weeks to monitor progress and adjust treatment as needed.
Questions To Ask Your Dermatologist
-
Is prescription azelaic acid safe for my trimester?
-
Which concentration is appropriate for my skin type and melasma severity?
-
Can I combine this with vitamin C or niacinamide?
-
When are postpartum treatments appropriate?
Clear questions lead to clearer outcomes.
Coordinating Care
Always inform both your dermatologist and OB-GYN about all skincare products and prescriptions.
According to the American College of Obstetricians and Gynecologists, coordination between dermatology and obstetric care is essential to manage pregnancy-related skin conditions safely. Your healthcare team should work together to support both your skin health and your baby’s well-being.
Azelaic Acid Vs. Other Pregnancy Melasma Treatments
Azelaic acid is the most balanced, pregnancy-safe melasma treatment, offering clinically proven pigment reduction with no known fetal risk. Unlike hydroquinone or retinoids, it combines safety, effectiveness, and versatility—making it the first-line option dermatologists recommend during pregnancy for managing melasma while protecting maternal and fetal health.
Let’s break down the comparison so you can see precisely why dermatologists consistently recommend azelaic acid as first-line therapy.
| Treatment | Pregnancy Safe? | Effectiveness | Speed of Results | Cost |
|---|---|---|---|---|
| Azelaic Acid 20% | ✅ Yes | High | 8-12 weeks | $$ |
| Hydroquinone | ❌ No | Very High | 4-8 weeks | $$ |
| Retinoids | ❌ No | High | 12+ weeks | $$$ |
| Vitamin C | ✅ Yes | Moderate | 12+ weeks | $$ |
| Kojic Acid | ⚠️ Limited data | Moderate | 8-12 weeks | $ |
| Glycolic Acid Peels | ⚠️ Use cautiously | Moderate | 6-8 weeks | $$$ |
| Natural Remedies | ✅ Yes | Low | Months | $ |
Why Azelaic Acid Wins For Pregnancy
Azelaic acid offers the rare combination of efficacy, safety, and multi-tasking benefits. It inhibits tyrosinase, reduces inflammation, treats pregnancy acne, and improves redness—all with minimal systemic absorption. Dr. Julie Karen, MD, notes that it’s her preferred choice for pregnant patients due to its “reliable results and reassuring safety profile.”
Its accessibility matters too: OTC options allow gradual entry before prescription escalation.
Clinical research published in Dermatologic Therapy demonstrates that 20% azelaic acid produces significant improvement in melasma, comparable to 4% hydroquinone, without the safety concerns.
Postpartum Options
After delivery, treatment choices expand. Azelaic acid remains safe during breastfeeding per the American Academy of Pediatrics guidance on topical medications.
If melasma persists, postpartum options include prescription hydroquinone, stronger chemical peels, and pigment-targeting lasers. Dr. Seemal Desai, MD, emphasizes that postpartum hormonal stabilization improves outcomes.
Key takeaway: Start safe during pregnancy. Escalate only if needed—often, consistency wins without aggressive intervention.
Frequently Asked Questions About Azelaic Acid and Pregnancy Melasma
Can I Use Azelaic Acid in My First Trimester?
Yes. Azelaic acid is FDA Pregnancy Category B and has minimal systemic absorption. Available evidence shows no fetal risk when used topically as directed. While melasma often appears later in pregnancy, azelaic acid may be used in the first trimester with OB-GYN approval.
How Long Can I Safely Use Azelaic Acid While Pregnant?
Azelaic acid can be used throughout pregnancy and while breastfeeding. There is no defined maximum duration, and long-term use (6–9 months or longer) has not shown safety concerns. Consistent use is often necessary for managing pregnancy-related melasma effectively.
Is 20% Azelaic Acid Too Strong for Pregnancy?
No. Prescription-strength 20% azelaic acid is considered pregnancy-safe. However, pregnant skin is more sensitive, so many patients tolerate 10–15% better initially. Concentration affects effectiveness and the risk of irritation, not fetal safety. You can increase strength gradually if needed.
Can I Use Azelaic Acid With Other Pregnancy-Safe Acne Treatments?
Yes. Azelaic acid is safe for treating both melasma and acne during pregnancy. It pairs well with niacinamide and gentle cleansers. Benzoyl peroxide may be used cautiously, but layering multiple exfoliating acids should be avoided to reduce irritation during pregnancy.
Can I Get Chemical Peels for Melasma While Pregnant?
Yes, but only low-strength peels under professional supervision. Glycolic acid (10–25%) and lactic acid (20–30%) are generally considered safe. Avoid salicylic acid, TCA, phenol peels, and other aggressive treatments until the postpartum period.
What If Azelaic Acid Doesn’t Work for My Melasma?
First, confirm correct use for at least 12 weeks with strict sun protection. Many failures are due to UV exposure or premature stopping. If results remain limited, a dermatologist can assess pigment depth and recommend prescription strength, combination therapy, or postpartum options.
Does Azelaic Acid Work on All Skin Tones?
Yes, azelaic acid is safe and effective for all skin tones, including darker complexions prone to melasma. It’s particularly beneficial for melanin-rich skin because it normalizes melanin production without causing hypopigmentation or white spots. Darker skin tones, while more susceptible to melasma, are at a lower risk of post-inflammatory hyperpigmentation than lighter skin tones with aggressive treatments.
What Results Can You Realistically Expect From Azelaic Acid During Pregnancy?
After nearly two decades working in medical and cosmetic science, I’ve learned that azelaic acid results during pregnancy are rarely dramatic—but they are meaningful. Real-world outcomes show gradual lightening, prevention of worsening melasma, and emotional relief. When paired with daily sunscreen and patience, azelaic acid delivers steady, evidence-aligned improvement without compromising pregnancy safety.
Success Story Examples
Example 1: “I developed melasma around week 20 of my pregnancy. My dermatologist prescribed 15% azelaic acid cream. The first week, I experienced some tingling and flaking, but by week 8, I noticed my forehead patches were definitely lighter. I religiously wore SPF 50 every single day—even indoors. It didn’t disappear completely during pregnancy, but it stopped getting worse. Three months postpartum, my skin is almost back to normal. I’m so glad I started treatment early!” — Sarah M., 32, first-time mom
Example 2: “I waited until my third trimester to start azelaic acid because I was nervous about using anything. I wish I’d started sooner! I used 10% from the drugstore and while it helped a little, the real improvement came after delivery when my hormones settled. The key lesson: be patient and don’t skip sunscreen. Ever.” — Priya K., 28, mother of two
Example 3: “My melasma was so dark on my upper lip that I felt like people were staring at me constantly. Started 20% prescription azelaic acid at 22 weeks. The initial dryness was challenging, but I powered through with a good moisturizer. By week 10, my patches had lightened maybe 30-40%—not gone, but so much better. The emotional relief of seeing progress was honestly as important as the physical improvement. Still using it postpartum and my skin looks better than it has in a year.” — Jessica L., 35, second pregnancy
Common Themes From User Experiences
Three factors determine success more than concentration:
-
Consistency: Daily 10–15% use outperforms sporadic 20% use
-
Sun Protection: UV exposure predicts treatment failure
-
Hormonal Timing: Postpartum fading accelerates as estrogen stabilizes
Dr. Pearl Grimes notes that hormonal normalization is critical to resolving melasma.
Realistic Expectations Vs. Marketing Hype
-
Timeline: 8–12 weeks for visible improvement, not days
-
Outcome: Control and lightening, not instant clearance
-
Science: About 70% of pregnancy melasma fades within one year postpartum.
Azelaic acid works best as part of a routine—not a miracle product, but a reliable one.
Conclusion
Azelaic acid stands as the gold standard for pregnancy melasma treatment—FDA Category B, clinically proven, and backed by decades of safe use. After years of formulating skincare protocols, I’ve seen that success requires three pillars: consistent azelaic acid application (10-20%), religious SPF 50+ sun protection, and patience through the 8-12 week treatment timeline.
Start with a patch test, apply to dehydrated skin twice daily, and pair with vitamin C for enhanced results. If over-the-counter options don’t deliver improvement after 12 weeks, consult your dermatologist for prescription-strength alternatives. Most importantly, continue treatment postpartum when hormonal normalization accelerates fading.
You’re joining 50-70% of pregnant women navigating this condition. While melasma may feel discouraging now, most cases improve significantly within a year postpartum. Your proactive approach—prioritizing both efficacy and safety—sets the foundation for clearer skin ahead.
Trust the process, protect your skin daily, and remember: you’re doing everything right.
Medical Disclaimer
The information provided in this article is for educational and informational purposes only
and is not intended as medical advice, diagnosis, or treatment. Skincare needs during
pregnancy vary by individual, and what works for one person may not be appropriate for another.
Always consult your obstetrician, dermatologist, or qualified healthcare professional before
starting, stopping, or combining any skincare products or treatments during pregnancy or
breastfeeding. This content does not replace personalized medical guidance, professional
evaluation, or clinical judgment.
📋 Medical Disclaimer
For Educational Purposes Only: This article is written by Kousar Subhan, a Medical Writer and Researcher, and is intended for informational and educational purposes only. The content provided is based on scientific research, peer-reviewed studies, and dermatological literature available as of December 2025.
Not Medical Advice: The information in this article does not constitute medical advice, diagnosis, or treatment recommendations. It should not be used as a substitute for professional medical consultation, diagnosis, or treatment from a board-certified dermatologist or qualified healthcare provider.
Individual Results May Vary: Skin conditions, including hyperpigmentation, melasma, and UV-induced pigmentation, vary significantly between individuals based on genetics, skin type, hormonal factors, and environmental exposure.
Consult Your Healthcare Provider: Before starting any new skincare regimen, especially if you are pregnant, breastfeeding, have diagnosed skin conditions, are taking medications, have sensitive skin, or are undergoing dermatological treatments.
Product Safety: Always perform a patch test before using new skincare products. Discontinue use and consult a healthcare professional if you experience irritation or adverse reactions.