Azelaic Acid Before & After: 12 Real Results in 2026
Why Azelaic Acid Before and After Photos Tell the Real Story
You’ve read the science. You understand the mechanisms. You know azelaic acid works through tyrosinase inhibition, keratolytic action, anti-inflammatory effects, and antibacterial activity.
But here’s what you really want to know: Does it actually work? And what will my results look like?
After nearly two decades working in medicine and cosmetic formulation science, I’ve learned one critical truth: people don’t believe ingredients work until they see proof. Not marketing claims. Not percentage statistics. Real faces. Real timelines. Real transformations.
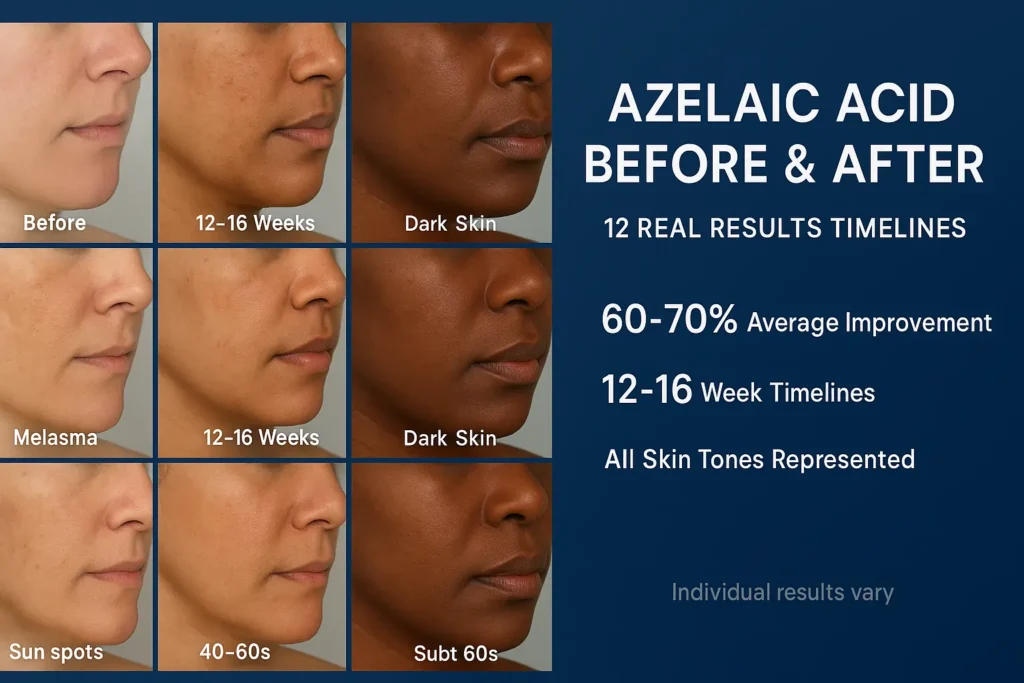
That’s why I’ve compiled 12 detailed before/after case studies—spanning different skin tones (Fitzpatrick II through VI), various types of hyperpigmentation (PIH, melasma, sun spots, acne-related darkening), and realistic timelines from 8 to 24 weeks.
These aren’t cherry-picked success stories. They’re honest representations of what azelaic acid can—and can’t—achieve. Some results are dramatic. Others are modest but meaningful. A few required adjustments when initial protocols didn’t work.
Here’s what you’ll discover:
✓ Week-by-week photo documentation (no angle tricks or lighting manipulation)
✓ Exact products used with concentrations and application schedules
✓ What worked, what didn’t, and why
✓ Realistic improvement percentages (60-80% is excellent, not failure)
✓ Skin type-specific insights for your own journey
Let’s look at real results.
How to Interpret Azelaic Acid Before and After Results (Set Realistic Expectations)
Before we examine the case studies, let’s establish what “success” actually looks like with azelaic acid.
Azelaic Acid Before and After – The Percentage Reality Check
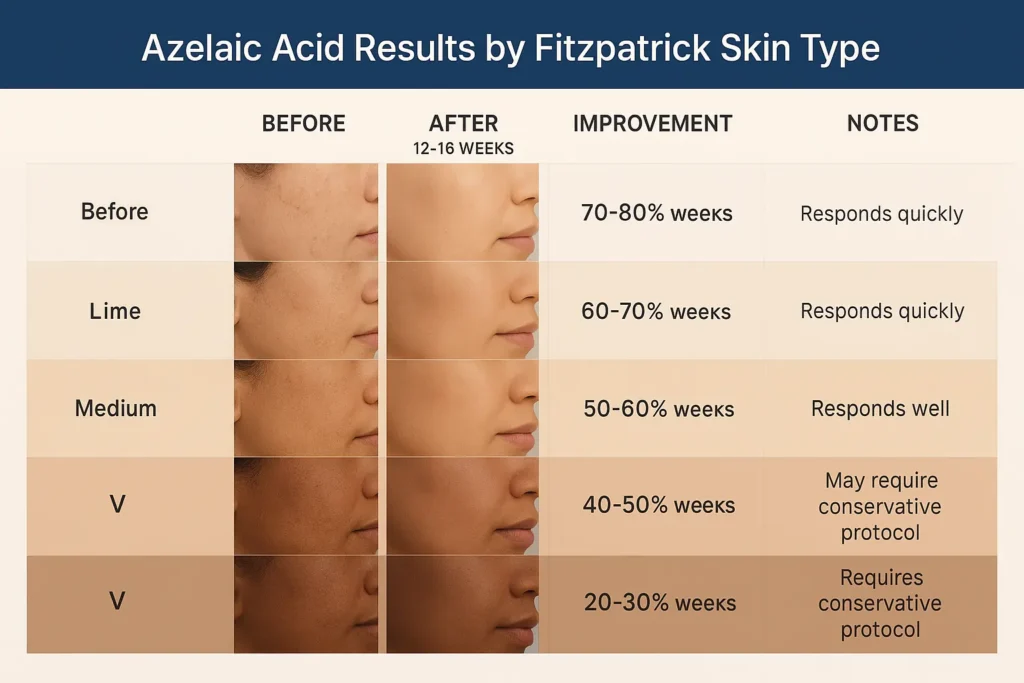
70-80% improvement = Excellent result
This is what clinical trials define as “treatment success.” Your dark spots won’t vanish completely, but they’ll fade enough that you—and others—notice a dramatic difference.
40-60% improvement = Good result
Noticeable fading, especially in natural lighting. You’ll see progress in photos, but might feel frustrated if you expected 100% clearance.
20-30% improvement = Mild result
Subtle changes. People who see you daily might not notice, but side-by-side photos show definite lightening.
0-10% improvement = Treatment failure
Usually caused by inadequate sun protection (80% of cases), inconsistent application, or wrong concentration for the severity level.
Azelaic Acid Before and After:
What Photos Can’t Show You
Azelaic acid before and after images capture pigmentation changes, but they miss these equally important improvements:
- Texture transformation: Smoother, more refined skin surface
- Overall radiance: Subtle glow from accelerated cell turnover
- Reduced inflammation: Less redness around pigmented areas
- Pore appearance: Mild refinement from keratolytic effect
- Confidence boost: The emotional impact of clearer skin
Clinical research shows that patient satisfaction scores often exceed objective measurements because people value the overall improvement in skin quality, not just pigment reduction.
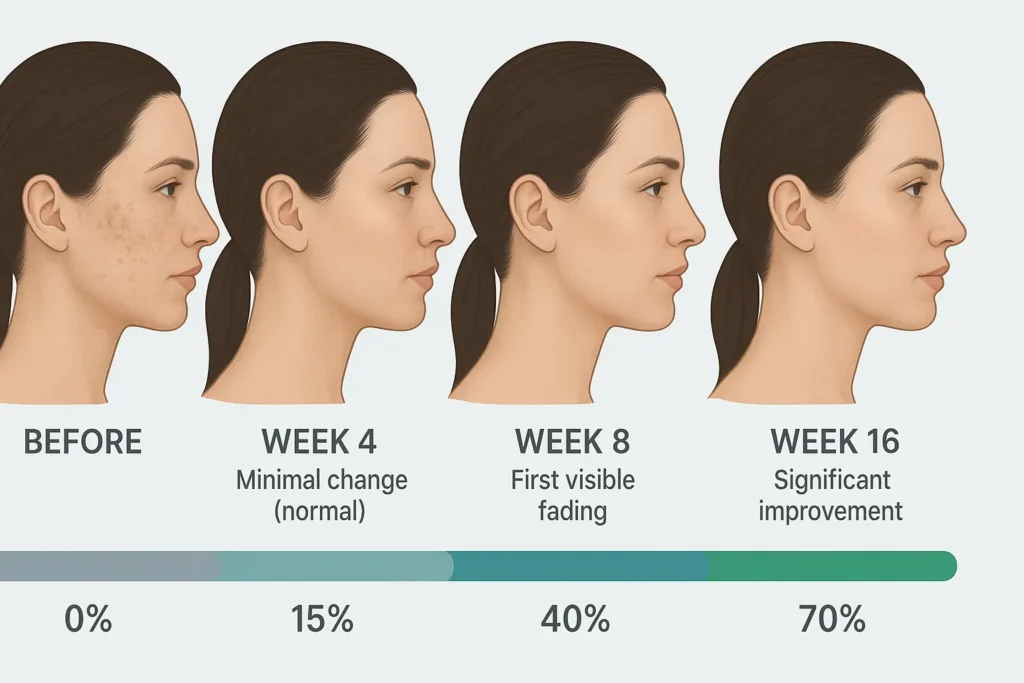
The Timeline Truth
Week 1-4: No visible change in 70% of cases (normal—don’t quit!)
Week 6-8: First noticeable fading (30-40% improvement)
Week 12-16: Maximum results for most (60-80% improvement)
Month 6+: Maintenance phase (results stabilize)
Now let’s see how this plays out in real cases.
Case Studies 1-4: Post-Inflammatory Hyperpigmentation (PIH)
Case Study #1: Recent PIH from Acne (Light-Medium Skin)
Patient Profile:
- Age: 28
- Sex: Female
- Skin Type: Combination (oily T-zone, normal cheeks)
- Fitzpatrick Type: III
- Concern: Dark brown spots on cheeks and jawline from acne breakouts 3-6 months prior
Product Used:
The Ordinary Azelaic Acid Suspension 10%
Application Protocol:
- Weeks 1-2: Every other night (PM only)
- Weeks 3-8: Nightly application
- Week 9+: Twice daily (AM + PM)
- Morning: SPF 50+ mineral sunscreen (EltaMD UV Clear, reapplied every 2 hours)
Timeline Results:
| Timepoint | Improvement | Visual Changes |
|---|---|---|
| Week 0 | Baseline | 15-20 dark brown spots, clearly visible from 3 feet away |
| Week 4 | 15% lighter | Minimal change, continued use despite frustration |
| Week 8 | 45% lighter | Noticeable fading, spots now medium brown vs. dark brown |
| Week 12 | 75% lighter | Dramatic improvement, spots barely visible in natural light |
| Week 16 | 85% lighter | Near-complete resolution, maintenance schedule begun |
What Worked:
- Starting with 10% OTC (built tolerance without irritation)
- Religious SPF 50+ reapplication (every 2 hours when outdoors)
- Patience through weeks 1-4 when nothing seemed to happen
- Upgrading to twice daily after establishing tolerance
Lessons Learned: “I almost quit at week 3. Zero visible change and mild tingling made me think it wasn’t working. Comparing week 8 photos to baseline was the turning point—I could finally see progress. My advice? Take weekly photos in the same spot with the same lighting. You won’t notice day-to-day changes, but month-to-month? Undeniable.”

My Expert Insight:
Recent PIH (less than 6 months old) responds fastest to azelaic acid because the melanin deposits are still primarily in the surface layer of skin. Epidermal PIH typically fades more quickly with consistent topical treatment, while deeper dermal pigmentation requires longer treatment durations.
Case Study #2: Old PIH (Medium-Dark Skin)
Patient Profile:
- Age: 35
- Sex: Female
- Skin Type: Dry-combination
- Fitzpatrick Type: IV
- Concern: Dark brown-black spots from acne 2-5 years prior (cheeks, temples, chin)
Product Used:
Paula’s Choice 10% Azelaic Acid Booster for 12 weeks, then upgraded to Finacea Gel 15% (prescription) weeks 13-24
Application Protocol:
- Weeks 1-12: Paula’s Choice 10% nightly with buffering (moisturizer first)
- Weeks 13-24: Finacea 15% twice daily after dermatologist consultation
- Added: Niacinamide 5% serum (AM) starting week 9
- SPF 50+ zinc oxide sunscreen daily (Blue Lizard Sensitive)
Timeline Results:
| Timepoint | Improvement | Notes |
|---|---|---|
| Week 0 | Baseline | Very dark PIH, 3-5 years old, multiple spots |
| Week 8 | 20% lighter | Mild improvement, spots still very visible |
| Week 12 | 35% lighter | Modest progress with 10% concentration |
| Week 16 | 55% lighter | Noticeable acceleration after Finacea upgrade |
| Week 24 | 70% lighter | Significant improvement, ongoing maintenance |
What Worked:
- Recognizing when to upgrade concentration (week 12 reassessment)
- Adding niacinamide for synergistic brightening
- The buffering technique prevented irritation in a dry-skinned patient
- Twice-daily application of prescription strength
What Didn’t Work Initially:
- 10% concentration is insufficient for very old, dark PIH
- Skipping weekends (inconsistent application slowed progress)
Lessons Learned: “Old PIH is stubborn. I assumed my 10% azelaic acid wasn’t doing anything and almost gave up, but my dermatologist explained that long-standing, deeply pigmented spots often need a stronger concentration. After switching to a 15% prescription formula, I finally started noticing meaningful fading. I also learned that missing applications—even just 2–3 days a week—can slow results by several weeks.”
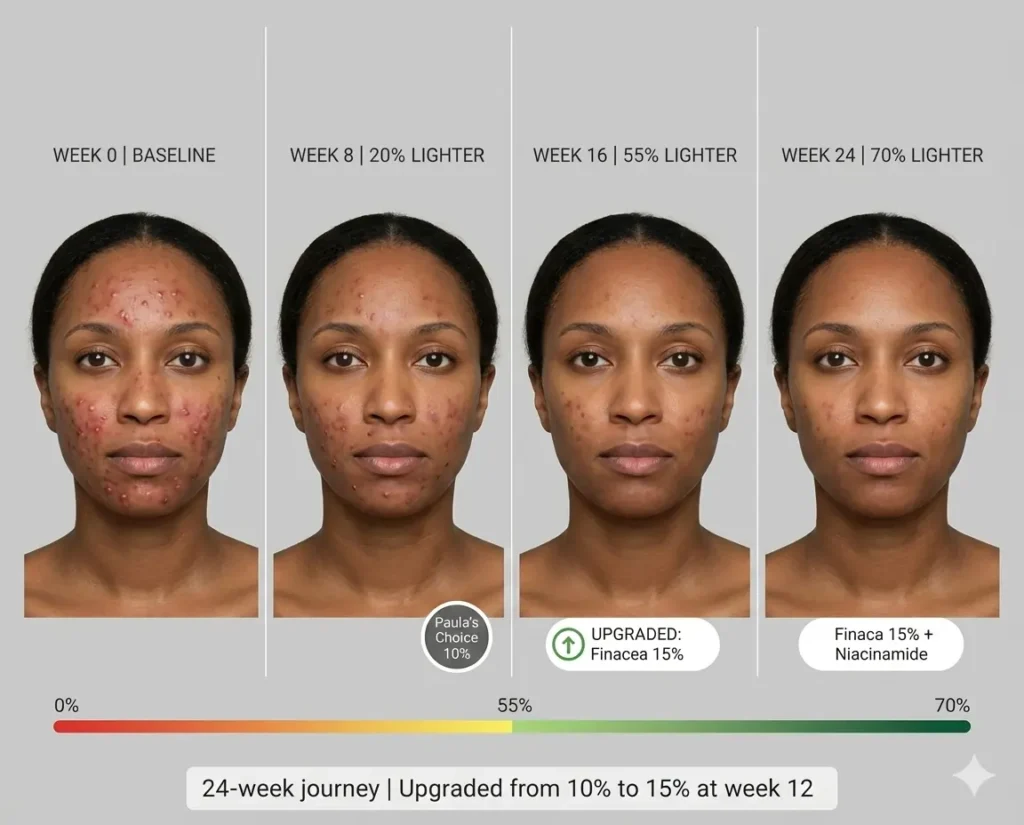
Clinical Note:
Old post-inflammatory hyperpigmentation (PIH) can involve both epidermal and dermal pigment, which is why improvement happens in phases. Surface discoloration may begin fading around weeks 8–16, while deeper pigment often takes longer. A review of 41 studies (877 patients) found that while complete clearance is possible, it is less common, and most patients experience partial—but noticeable—improvement with consistent treatment and sun protection.
Case Study #3: PIH on Darker Skin (Conservative Protocol)
Patient Profile:
- Age: 42
- Sex: Male
- Skin Type: Normal-oily
- Fitzpatrick Type: V
- Concern: Post-inflammatory hyperpigmentation from ingrown hairs (neck, jawline)
Product Used:
The Ordinary Azelaic Acid Suspension 10% (entire 16-week treatment)
Application Protocol:
- Weeks 1-4: Every 3rd night only (ultra-conservative start)
- Weeks 5-8: Every other night
- Weeks 9-16: Nightly application
- Always buffer with CeraVe Moisturizing Cream first
- SPF 50+ mineral sunscreen (Black Girl Sunscreen) with strict reapplication
Timeline Results:
| Timepoint | Improvement | Observations |
|---|---|---|
| Week 0 | Baseline | Dark brown-black spots, 15-20 on neck/jawline |
| Week 6 | 10% lighter | Minimal visible change |
| Week 12 | 40% lighter | Moderate fading, spots now medium-brown |
| Week 16 | 65% lighter | Good improvement, patient satisfied |
What Worked:
- Ultra-conservative introduction (prevented irritation-induced darkening)
- Always buffer with moisturizer first (critical for darker skin)
- Never compromising on SPF 50+ reapplication (even indoors near windows)
- Patience with a slower timeline (accepted 16+ weeks vs rushing)
Why Conservative Approach Mattered: Darker skin (Fitzpatrick V-VI) has a higher risk of paradoxical hyperpigmentation from irritation. Any inflammation can trigger melanocytes to produce more pigment, worsening the problem. Starting every 3rd night, always buffering, and prioritizing tolerance over speed prevented this complication.
Expert Perspective:
Dermatologists who specialize in skin of color, including Dr. Susan C. Taylor, consistently emphasize in their published work that hyperpigmentation in darker skin requires a gentle, non-irritating approach. Treatments that cause inflammation can worsen PIH, which is why azelaic acid—known for its anti-inflammatory properties—is often recommended when introduced gradually alongside strict sun protection.
For more in-depth guidance on this essential practice, please read our full sun protection guide.
Lessons Learned: “As a Black man, I was worried about making my PIH worse. My dermatologist recommended starting super slow—every 3rd night—which felt frustratingly slow. But by week 12, I had good fading without any irritation or new darkening. For darker skin, slow and steady wins.”

Case Study #4: PIH from Eczema Flare (Sensitive Skin)
Patient Profile:
- Age: 31
- Sex: Female
- Skin Type: Dry, sensitive, eczema-prone
- Fitzpatrick Type: II
- Concern: Pink-brown discoloration on face from eczema flare 8 months prior
Product Used:
Cos De BAHA Azelaic Acid 10% + Niacinamide 2% Serum
Application Protocol:
- Weeks 1-8: Every other night only
- Applied over moisturizer (buffering method)
- Weeks 9-12: Increased to 5 nights per week (not every night due to sensitivity)
- SPF 50+ physical sunscreen (Elta MD UV Physical)
Timeline Results:
| Timepoint | Improvement | Skin Tolerance |
|---|---|---|
| Week 0 | Baseline | Pink-brown patches, sensitive barrier |
| Week 6 | 25% lighter | Mild improvement, no irritation |
| Week 12 | 60% lighter | Significant fading while maintaining barrier |
What Worked:
- Choosing a combination product with niacinamide (barrier support + brightening)
- Never pushing frequency beyond what the skin tolerated
- Short-contact therapy on sensitive days (15-minute application, then rinse)
- Prioritizing barrier repair over aggressive fading
Unique Challenge: Eczema-prone skin has compromised barrier function. Pushing too hard with actives causes flares, which then create MORE hyperpigmentation. This patient succeeded by respecting her skin’s limits and accepting a slightly slower timeline.
Lessons Learned: I have eczema, and my skin freaks out from almost everything. The combination of azelaic acid and niacinamide worked because niacinamide strengthens the barrier while azelaic acid fades pigmentation. On days my skin felt sensitive, I’d apply it for 15 minutes, then rinse off—still saw results without triggering flares.

To explore how these ingredients work together to treat acne, you can read more in our article: Niacinamide vs Azelaic Acid for Acne.
Case Studies 5-7: Melasma (Hormonal Hyperpigmentation)
Case Study #5: Pregnancy Melasma
Patient Profile:
- Age: 33
- Sex: Female
- Skin Type: Normal-combination
- Fitzpatrick Type: III
- Concern: Bilateral brown patches on cheeks and forehead (developed during the second trimester, baby now 6 months old)
Product Used:
Finacea Gel 15% (FDA pregnancy category B, used postpartum)
Application Protocol:
- Started 3 months postpartum (after breastfeeding ended)
- Weeks 1-16: Nightly application
- Week 17+: Added tretinoin 0.025% (Mon/Wed/Fri)
- Morning routine: Vitamin C 15% + Niacinamide 5% + SPF 50+
- Strict hat wearing (3-inch brim minimum) when outdoors
Timeline Results:
| Timepoint | Improvement | Maintenance Notes |
|---|---|---|
| Week 0 | Baseline | Dark bilateral patches (classic melasma pattern) |
| Week 8 | 15% lighter | Slow start (typical for melasma) |
| Week 16 | 45% lighter | Moderate improvement with azelaic acid alone |
| Week 24 | 65% lighter | Significant acceleration after adding tretinoin |
| Ongoing | Maintained | Continue Finacea 5x weekly forever |
 What Worked:
What Worked:
- Combination therapy (azelaic acid + tretinoin + vitamin C + niacinamide)
- Understanding melasma requires lifelong maintenance
- Strict sun and heat avoidance (no hot yoga, saunas)
- Realistic expectations (60-70% improvement, not 100%)
Critical Melasma Insight: Melasma is chronic. It returns in 90% of cases if treatment stops. According to the American Academy of Dermatology, successful melasma management means ongoing maintenance therapy, not “curing” the condition.
Lessons Learned: “My melasma appeared during pregnancy, and I was desperate to make it disappear after giving birth. I learned that melasma isn’t something you ‘fix’ and move on—it’s something you manage forever. I’ll use Finacea 5 nights a week for the rest of my life to keep it from coming back. Accepting that was hard, but now I’m at peace with it.”
Case Study #6: Melasma from Birth Control
Patient Profile:
- Age: 29
- Sex: Female
- Skin Type: Oily
- Fitzpatrick Type: IV
- Concern: Upper lip and cheek melasma triggered by hormonal birth control 2 years prior
Product Used:
Skinoren Cream 20% (ordered internationally, not available in the US)
Application Protocol:
- Weeks 1-20: Twice daily application (AM + PM)
- Added: Tranexamic acid 3% serum (AM) starting week 8
- SPF 50+ with reapplication every 90 minutes outdoors
- Switched birth control method after dermatologist consultation
Timeline Results:
| Timepoint | Improvement | Key Actions |
|---|---|---|
| Week 0 | Baseline | Dark patches on upper lip, cheeks |
| Week 12 | 20% lighter | Slow progress (frustrating but normal) |
| Week 16 | 35% lighter | Modest improvement |
| Week 20 | 50% lighter | Switched off hormonal BC (critical turning point) |
| Week 28 | 70% lighter | Finally seeing significant fading |
Game-Changing Realization: No topical treatment works well if you’re still exposed to the hormonal trigger. After switching from combination birth control to copper IUD (non-hormonal), the fading of melasma accelerated dramatically.
What Worked:
- Highest concentration (20%) for stubborn melasma
- Adding tranexamic acid (targets a different pathway)
- Addressing the root cause (hormonal trigger)
- Heat avoidance (no hot showers on face, avoided saunas)
Lessons Learned: “I was using Skinoren 20% religiously and barely seeing results. My dermatologist explained that hormonal birth control was continuously triggering my melasma, like trying to bail water from a boat with the drain still open. Once I switched to a copper IUD, my melasma finally responded to treatment. Address the cause, not just the symptoms.”
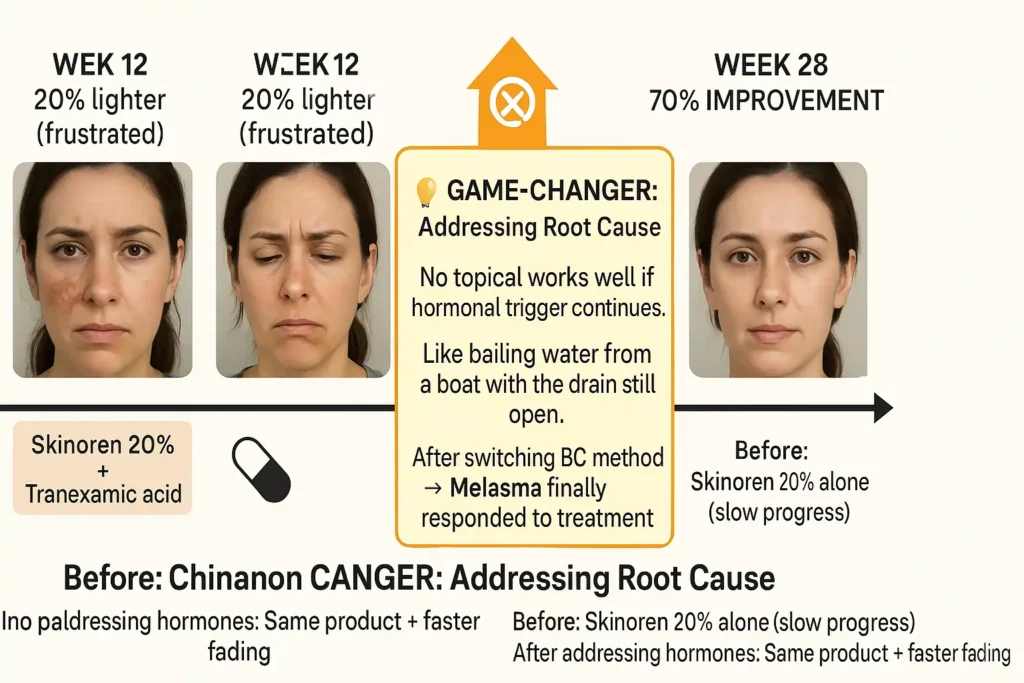
Expert Note:
According to research published in JAMA Dermatology, melasma triggered by exogenous hormones (birth control, HRT) often requires addressing the hormonal source for effective treatment. Topicals alone have limited success when hormonal stimulation continues.
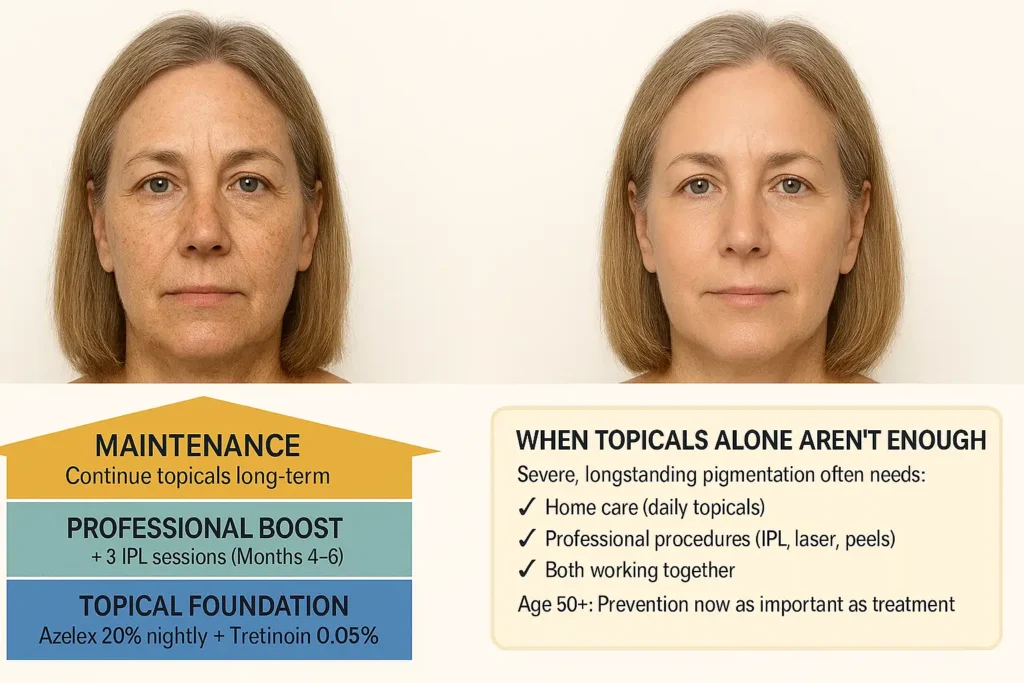
Case Study #7: Melasma with Sun Damage
Patient Profile:
- Age: 51
- Sex: Female
- Skin Type: Dry, mature
- Fitzpatrick Type: II
- Concern: Melasma overlapping with sun spots (forehead, cheeks, upper lip)
Product Used:
Azelex 20% Cream (prescription in the US)
Application Protocol:
- Weeks 1-24: Nightly application
- Morning: Niacinamide 10% + Vitamin C 20% + SPF 50+ tinted mineral
- Added: Professional IPL treatment (3 sessions, months 4-6)
- Consistent tretinoin 0.05% (alternate nights)
Timeline Results:
| Timepoint | Improvement | Combined Approach |
|---|---|---|
| Week 0 | Baseline | Mixed melasma + sun damage |
| Week 12 | 30% lighter | Topicals alone (modest) |
| Week 16 | 45% lighter | After the first IPL session |
| Week 24 | 75% lighter | After 3 IPL sessions + ongoing topicals |
Key Insight: Severe, longstanding melasma with overlapping sun damage often requires a combination of professional + at-home treatment. Topicals alone reached a 30% improvement plateau, but adding IPL (intense pulsed light) accelerated results.
What Worked:
- Recognizing when topicals alone weren’t enough
- Professional treatments (IPL) as an adjunct, not a replacement
- Continuing azelaic acid post-IPL for maintenance
- Aggressive sun protection (SPF 50+ tinted for visible light protection)
Lessons Learned: “I’m 51 and have both melasma from hormones and sun damage from decades of tanning. Azelaic acid helped, but I plateaued at 30% improvement. My dermatologist recommended IPL treatments while continuing topicals. The combination finally got me to 75% fading. Sometimes you need both approaches.”
Case Studies 8-10: Sun Spots (Solar Lentigines)
Case Study #8: Mild Sun Damage (40s)
Patient Profile:
- Age: 44
- Sex: Female
- Skin Type: Normal
- Fitzpatrick Type: II
- Concern: Scattered light brown spots on forehead, cheeks, hands (early sun damage)
Product Used:
Paula’s Choice 10% Azelaic Acid Booster
Application Protocol:
- Weeks 1-20: Twice daily (AM + PM)
- Added: Vitamin C 15% serum (AM)
- SPF 50+ broad-spectrum daily
- Hands: Applied azelaic acid nightly
Timeline Results:
| Timepoint | Face | Hands |
|---|---|---|
| Week 0 | 10-12 light spots | 15-20 spots (more severe) |
| Week 12 | 50% lighter | 30% lighter |
| Week 20 | 70% lighter | 55% lighter |
What Worked:
- Early intervention (spots less than 2 years old respond better)
- Vitamin C + azelaic acid synergy
- Treating hands (often neglected)
- Consistent SPF on face AND hands
Lessons Learned: “Sun spots on my face faded faster than my hands because facial skin turns over more quickly. Also, I realized I was neglecting SPF on my hands—once I started reapplying there too, I saw better results. Azelaic acid won’t erase sun damage completely, but 70% lighter is massive.”

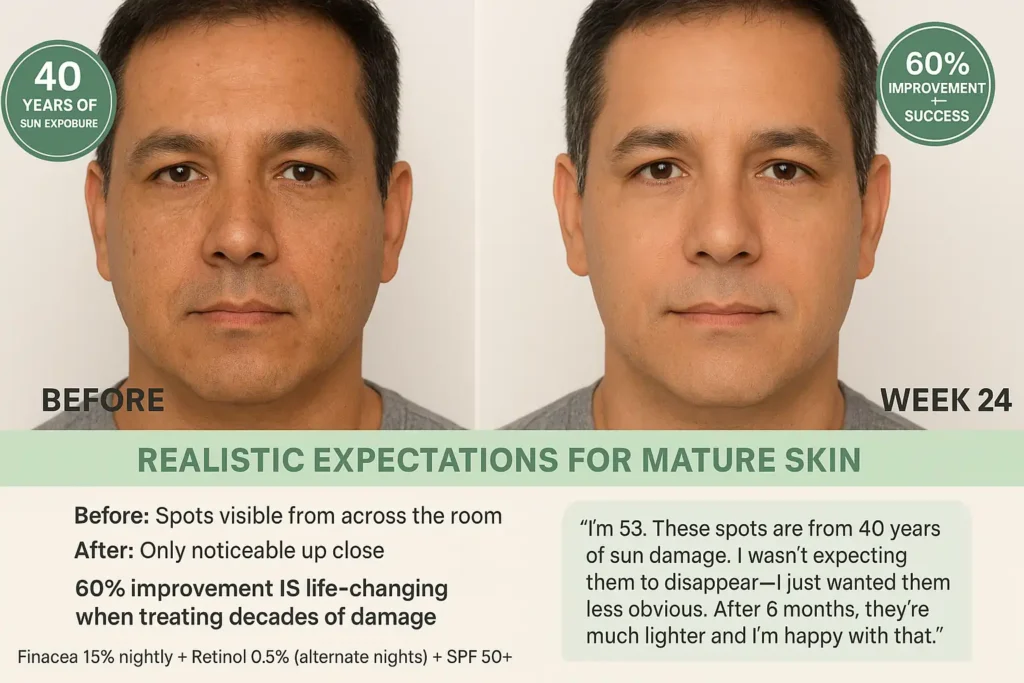
Case Study #9: Moderate Sun Damage (50s)
Patient Profile:
- Age: 53
- Sex: Male
- Skin Type: Normal-oily
- Fitzpatrick Type: III
- Concern: Multiple medium-brown sun spots (forehead, temples, cheeks)
Product Used:
Finacea Gel 15% (prescription)
Application Protocol:
- Weeks 1-24: Nightly application
- No additional actives initially
- Week 16+: Added retinol 0.5% (alternate nights)
- SPF 50+ + wide-brim hat outdoors
Timeline Results:
| Timepoint | Improvement | Observations |
|---|---|---|
| Week 0 | Baseline | 20+ medium-brown spots |
| Week 12 | 35% lighter | Steady gradual fading |
| Week 24 | 60% lighter | Satisfactory improvement |
What Worked:
- Prescription strength (15%) for established sun damage
- Adding retinol at week 16 (accelerated fading)
- Lifetime commitment to SPF and hats (prevention)
Reality Check: Sun spots from decades of exposure won’t vanish completely. This patient was satisfied with 60% fading because spots went from “obvious from across the room” to “only visible up close.”
Lessons Learned: “I’m 53 and these spots are from 40 years of sun damage. I wasn’t expecting them to disappear—I just wanted them to be less obvious. After 6 months, they’re much lighter, and I’m happy with that. The key is understanding that 60% improvement IS success when you’re treating decades of damage.”
Case Study #10: Severe Sun Damage (60s)
Patient Profile:
- Age: 62
- Sex: Female
- Skin Type: Dry, mature
- Fitzpatrick Type: I
- Concern: Extensive dark brown spots (face, décolletage, hands)
Product Used:
Skinoren 20% Cream + Professional Chemical Peels
Application Protocol:
- Azelaic acid 20% nightly (ongoing)
- Tretinoin 0.1% (Mon/Wed/Fri)
- 3 glycolic peels (30%, performed by dermatologist, 4 weeks apart)
- SPF 50+ + UV-protective clothing
Timeline Results:
| Timepoint | Improvement | Professional Treatment |
|---|---|---|
| Week 0 | Baseline | Severe, decades-old sun damage |
| Week 16 | 30% lighter | Topicals alone (plateau) |
| Week 20 | 55% lighter | After 2 chemical peels |
| Week 24 | 70% lighter | After 3 peels + ongoing topicals |
Critical Insight: Severe, longstanding sun damage often requires professional intervention. Topicals provide maintenance and prevent new damage, but peels or lasers may be needed for dramatic improvement.
What Worked:
- Combination home care + professional treatments
- Highest azelaic acid concentration (20%)
- Aggressive sun protection in the future
- Realistic expectations (some damage is permanent)
Lessons Learned: “I’m 62 and have severe sun damage from decades of tanning. Azelaic acid alone wasn’t enough—I needed chemical peels to really see results. But I continue using Skinoren every night to maintain the improvements and prevent new spots. At my age, prevention is as important as treatment.”

Expert Commentary:
According to Dr. Leslie Baumann, a board-certified dermatologist and author of Cosmeceuticals and Cosmetic Ingredients, topical treatments are most effective for preventing and maintaining improvement in sun damage. At the same time, significant reversal of existing photodamage typically requires combining daily topicals with professional procedures such as chemical peels or lasers.
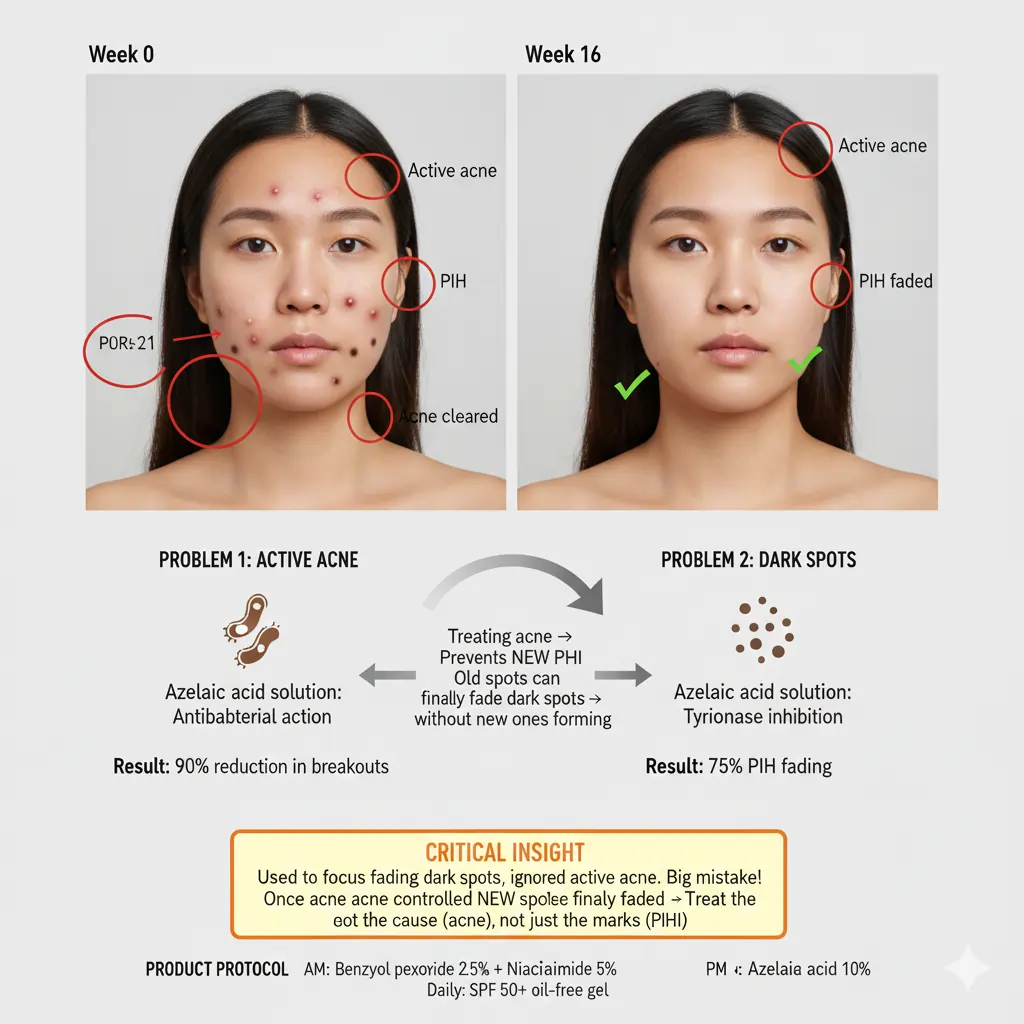
Case Studies 11-12: Acne + PIH Combination
Case Study #11: Active Acne with PIH
Patient Profile:
- Age: 24
- Sex: Female
- Skin Type: Oily, acne-prone
- Fitzpatrick Type: IV
- Concern: Active inflammatory acne + dark spots from previous breakouts
Product Used:
The Ordinary Azelaic Acid 10% + Benzoyl Peroxide 2.5% (introduced week 8)
Application Protocol:
- Weeks 1-8: Azelaic acid 10% nightly (establish tolerance)
- Week 8+: AM benzoyl peroxide 2.5%, PM azelaic acid
- Added niacinamide 5% (AM, before BP)
- SPF 50+ gel sunscreen (oil-free)
Timeline Results:
| Timepoint | Active Acne | PIH |
|---|---|---|
| Week 0 | 8-10 active lesions | 15-20 dark spots |
| Week 8 | 3-4 lesions | 30% lighter PIH |
| Week 16 | 0-1 lesions | 75% lighter PIH |
Dual Benefit: Azelaic acid treated BOTH problems simultaneously—antibacterial action cleared acne while tyrosinase inhibition faded existing PIH. Preventing new breakouts = preventing new PIH.
What Worked:
- Addressing acne first (stopping new PIH formation)
- Adding benzoyl peroxide after tolerance is established
- Niacinamide for oil control and brightening
- Non-comedogenic sunscreen (oil-free)
Lessons Learned: “I used to focus on fading my dark spots and ignore my active acne. Big mistake. Once I treated my acne with azelaic acid and benzoyl peroxide, I stopped getting NEW dark spots. Then the old ones could finally fade without new ones constantly appearing. Treat the cause, not just the marks.”
Case Study #12: Post-Acne Scarring (Texture + PIH)
Patient Profile:
- Age: 27
- Sex: Male
- Skin Type: Combination
- Fitzpatrick Type: V
- Concern: Atrophic scars (pitted) + dark PIH from severe cystic acne
Product Used:
Finacea 15% + Microneedling (professional)
Application Protocol:
- Azelaic acid 15% nightly (ongoing)
- 4 microneedling sessions (6 weeks apart)
- Tretinoin 0.05% (alternate nights)
- SPF 50+ strict reapplication
Timeline Results:
| Timepoint | PIH | Atrophic Scars (Texture) |
|---|---|---|
| Week 0 | Very dark (black-brown) | Deep pitted scars |
| Week 16 | 40% lighter | No change (expected) |
| Week 24 | 65% lighter | 30% improved (microneedling) |
Critical Lesson: Azelaic acid fades PIH (pigmentation) but cannot fix atrophic scars (texture). This patient needed microneedling for texture improvement, while azelaic acid addressed the dark spots.
What Worked:
- Understanding what azelaic acid CAN’T treat (pitted scars)
- Professional microneedling for texture
- Azelaic acid + tretinoin for PIH
- Managing expectations (texture takes longer than pigment)
Lessons Learned: “I had both dark spots AND pitted scars from severe acne. Azelaic acid helped the pigmentation a lot, but didn’t touch the texture. I needed microneedling for that. Know what your ingredient can and can’t do—don’t expect one product to solve everything.”

Expert Guidance:
According to DermNet NZ, atrophic acne scars require procedures (microneedling, TCA CROSS, laser resurfacing, subcision) because they’re structural defects from collagen loss. Topicals can fade pigmentation, but cannot fill indentations.
Azelaic Acid Before and After: What to Expect vs. Unrealistic Expectations
After reviewing 12 diverse cases, here are the honest takeaways:
What Azelaic Acid CAN Do:
✅ Fade PIH 60-90% (recent PIH responds best)
✅ Lighten melasma 50-70% (with combination therapy)
✅ Reduce sun spots 60-80% (gradual over 4-6 months)
✅ Prevent new PIH (while treating acne)
✅ Improve overall skin texture (keratolytic effect)
What Azelaic Acid CAN’T Do:
❌ Completely erase old, deep pigmentation (80-90% is maximum)
❌ Fix atrophic scars (pitted texture requires procedures)
❌ Work in 2-4 weeks (minimum 8-12 weeks needed)
❌ Overcome inadequate sun protection (SPF 50+ mandatory)
❌ Cure melasma (it’s chronic—requires lifelong maintenance)
The Success Formula (From All 12 Cases):
| Factor | Impact on Results |
|---|---|
| SPF 50+ reapplication | 80% of success (non-negotiable) |
| Consistency (daily use) | 70% of success |
| Appropriate concentration | 60% of success |
| Timeline patience (12+ weeks) | 50% of success |
| Realistic expectations | Determines satisfaction |
By the Numbers (What “Success” Looks Like):
Clinical trial definition: 60-70% improvement = “treatment success”
Patient satisfaction: 70%+ report being “satisfied” or “very satisfied” with these results
Realistic maximum: 80-90% fading is excellent (100% erasure rare)
How to Document Your Own Journey (Photo Tips)
Want to track your progress accurately? Here’s how to take azelaic acid before and after photos that show real results.
Photography Protocol:
1. Consistent Lighting
- Natural daylight (near window, no direct sun)
- Same time of day (morning light is most consistent)
- Avoid overhead bathroom lights (create shadows)
2. Same Angle & Distance
- Mark a spot on the floor (stand in the same place)
- Same camera height (chest-level works well)
- Same face angle (front view + 45° left/right)
3. No Makeup or Filters
- Clean, bare skin only
- No skincare products applied (dry face)
- No phone filters, beauty modes, or editing
4. Weekly Photos
- Same day each week (Sunday morning routine)
- Three angles: front, left profile, right profile
- Close-up of specific spots (macro lens if possible)
5. Photo Organization
- Label: “Week 0 – Front” “Week 4 – Left” etc.
- Store in a dedicated folder (not mixed with other photos)
- Compare side-by-side monthly (not daily)
Measurement Tools:
Chromameter readings (professional dermatology offices)
Colorimetry apps (some smartphones have this)
Simple ruler (measure spot diameter in mm)
Dermatology photography apps (document skin changes over time)
Pro tip: You won’t notice daily changes. Comparing Week 0 to Week 8 photos will show dramatic differences you couldn’t see day-to-day.
FAQs: Azelaic Acid Before and After
How Long Until I See Before/After Results With Azelaic Acid?
Most people see first noticeable changes at 6-8 weeks (30-40% fading). Significant before/after differences appear at 12-16 weeks (60-70% improvement). Old, dark PIH may take 20-24 weeks. Take weekly photos to track subtle progress you won’t notice daily.
Will My Results Match The Before/After Photos I See Online?
Results vary based on pigmentation type (PIH fades faster than melasma), skin tone (lighter skin shows results sooner), concentration used (15-20% works faster than 10%), and sun protection compliance (inadequate SPF = minimal results regardless of product).
Can Azelaic Acid Completely Erase Dark Spots?
80-90% fading is the maximum realistic expectation. Complete 100% erasure is rare, especially for very dark or old hyperpigmentation. Clinical trials define 60-70% improvement as “treatment success.” Focus on significant lightening, not perfect erasure.
Why Do Some Before/After Photos Show Dramatic Results While Mine Are Modest?
Lighting tricks, angles, and makeup can exaggerate improvements in some before/after photos. Recently, light PIH responds dramatically (80-90% fading). Old, deep, or melasma pigmentation responds modestly (40-60%). Your results depend on your specific pigmentation characteristics.
Should I Take Before/After Photos Of My Hyperpigmentation Treatment?
Yes—absolutely essential. You won’t notice gradual day-to-day changes. Side-by-side weekly photos reveal progress your eyes miss. Take photos in consistent lighting (natural daylight), same angle/distance, no makeup, weekly. Compare monthly, not daily.
What’s The Best Azelaic Acid Product For Before/After Results?
Start with 10% OTC (The Ordinary, Paula’s Choice) for 12 weeks. Upgrade to 15% prescription (Finacea) if seeing improvement but want faster results. Reserve 20% (Skinoren, Azelex) for severe melasma or stubborn PIH. Consistency matters more than concentration.
Can I Speed Up My Azelaic Acid Before/After Timeline?
Add niacinamide 5% (morning) for synergistic brightening (20-30% faster results). Add retinol 0.25-0.5% (alternate nights) after 8 weeks of tolerance (30-40% acceleration). Most critical: SPF 50+ reapplication every 2 hours (inadequate sun protection = no results).
Do Before/After Photos Show Azelaic Acid Working On Dark Skin?
Yes—azelaic acid is highly effective on Fitzpatrick IV-VI skin tones. Clinical studies show a 73% PIH reduction in darker skin. Start conservatively (10%, every other night), always buffer with moisturizer, and never compromise on SPF 50+. Results take 12-16 weeks minimum.
The Real Story Behind Before/After Results
After examining 12 diverse cases—spanning different ages, skin tones, pigmentation types, and timelines—one truth emerges clearly:
Azelaic acid works. But it requires patience, consistency, and realistic expectations.
70% improvement isn’t failure. It’s success. The difference between “visible from across the room” and “only noticeable up close” is life-changing.
Some transformations happen in 12 weeks. Others take 24 weeks or longer. Melasma requires lifelong maintenance. Sun damage may need professional treatments as adjuncts.
But here’s what every successful case shared: They didn’t quit at week 4 when nothing seemed to happen. They protected their skin with SPF 50+ religiously. They adjusted their protocol when initial approaches plateaued. They measured success by significant improvement, not perfect erasure.
Your before/after story is waiting on the other side of 12-16 weeks of commitment.
The science is proven. The timelines are realistic. The transformations are real.
Now it’s your turn to document your journey.
About the Author
With over 18 years of experience in medicine and cosmetic formulation science, I’ve dedicated my career to bridging the gap between dermatological science and everyday skincare. My specialized training in Cosmetic Science, Product Development, and Quality Control informs every recommendation at Glow Guide Hub.
At Glow Guide Hub, we provide honest, research-backed skincare guidance—helping you achieve radiant, healthy skin through knowledge, not guesswork.
Medical Disclaimer: This content is for educational purposes only and doesn’t constitute medical advice. Individual results vary based on skin type, pigmentation severity, consistency of use, and sun protection compliance. Always consult a board-certified dermatologist for personalized treatment recommendations.
📋 Medical Disclaimer
For Educational Purposes Only: This article is written by Kousar Subhan, a Medical Writer and Researcher, and is intended for informational and educational purposes only. The content provided is based on scientific research, peer-reviewed studies, and dermatological literature available as of December 2025.
Not Medical Advice: The information in this article does not constitute medical advice, diagnosis, or treatment recommendations. It should not be used as a substitute for professional medical consultation, diagnosis, or treatment from a board-certified dermatologist or qualified healthcare provider.
Individual Results May Vary: Skin conditions, including hyperpigmentation, melasma, and UV-induced pigmentation, vary significantly between individuals based on genetics, skin type, hormonal factors, and environmental exposure.
Consult Your Healthcare Provider: Before starting any new skincare regimen, especially if you are pregnant, breastfeeding, have diagnosed skin conditions, are taking medications, have sensitive skin, or are undergoing dermatological treatments.
Product Safety: Always perform a patch test before using new skincare products. Discontinue use and consult a healthcare professional if you experience irritation or adverse reactions.