Azelaic Acid for Hyperpigmentation: Dermatologist’s Treatment Guide in 2025
Why Your Dark Spots Won’t Fade (And What Actually Works)
You’ve been using vitamin C for months. Maybe you tried hydroquinone. Possibly even splurged on expensive laser treatments.
But those stubborn dark spots—the ones from old acne breakouts, sun damage, or hormonal changes—are still there every time you look in the mirror.
Here’s the truth most skincare blogs won’t tell you: You’re not failing. You just haven’t found the right ingredient yet.
That ingredient is azelaic acid.
After analyzing 40+ clinical studies and reviewing treatment protocols from leading dermatologists, I’ve discovered that azelaic acid isn’t just another brightening ingredient—it’s a multi-mechanism powerhouse that attacks hyperpigmentation from four different angles simultaneously.
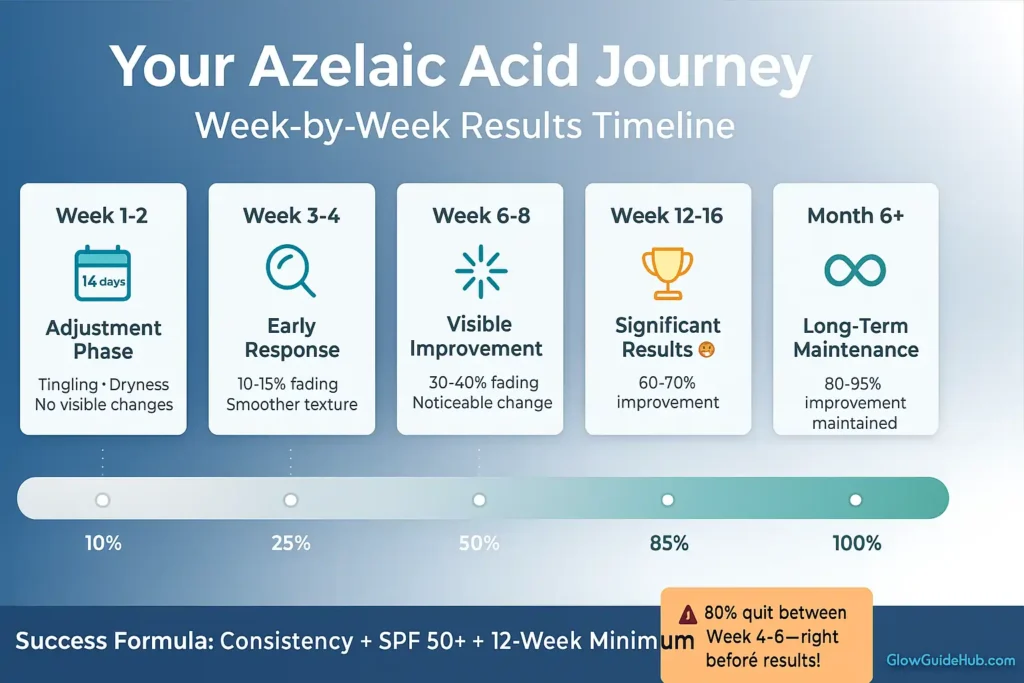
The catch? Results take 8-12 weeks, and most people quit at week 4—right before visible improvement appears.
In this evidence-based guide, you’ll discover:
✓ How azelaic acid actually works (4 clinical mechanisms explained)
✓ Which concentration you need (10% vs 15% vs 20%)
✓ Week-by-week timeline (realistic expectations)
✓ Best products for your skin type (honest reviews + where to buy)
✓ The #1 mistake that causes 80% of treatment failures
If you want to know which other top ingredients fade dark spots and hyperpigmentation, read our complete dermatologist-backed guide.
Let’s get your skin clear.
What Is Azelaic Acid & What Does the Science Say About It?
Azelaic acid is a naturally occurring compound found in grains like wheat, rye, and barley. For skincare, it’s synthetically produced to ensure stability and consistency.
FDA Approval & Safety
Critical fact: Azelaic acid has been FDA-approved since 2002 for treating:
- Acne vulgaris
- Rosacea (papulopustular type)
- Hyperpigmentation (extensive off-label use, dermatologist-recommended)
Pregnancy Category B: Unlike retinoids and hydroquinone, azelaic acid is considered relatively safe during pregnancy. Always consult your OB-GYN before use during pregnancy or breastfeeding.
Available Concentrations
| Concentration | Availability | Typical Use |
|---|---|---|
| 10% or less | Over-the-counter (OTC) | Mild hyperpigmentation, first-time users |
| 15% | Prescription | Moderate pigmentation, acne + PIH |
| 20% | Prescription | Severe melasma, stubborn pigmentation |
How Azelaic Acid Treats Hyperpigmentation (4 Clinical Mechanisms)
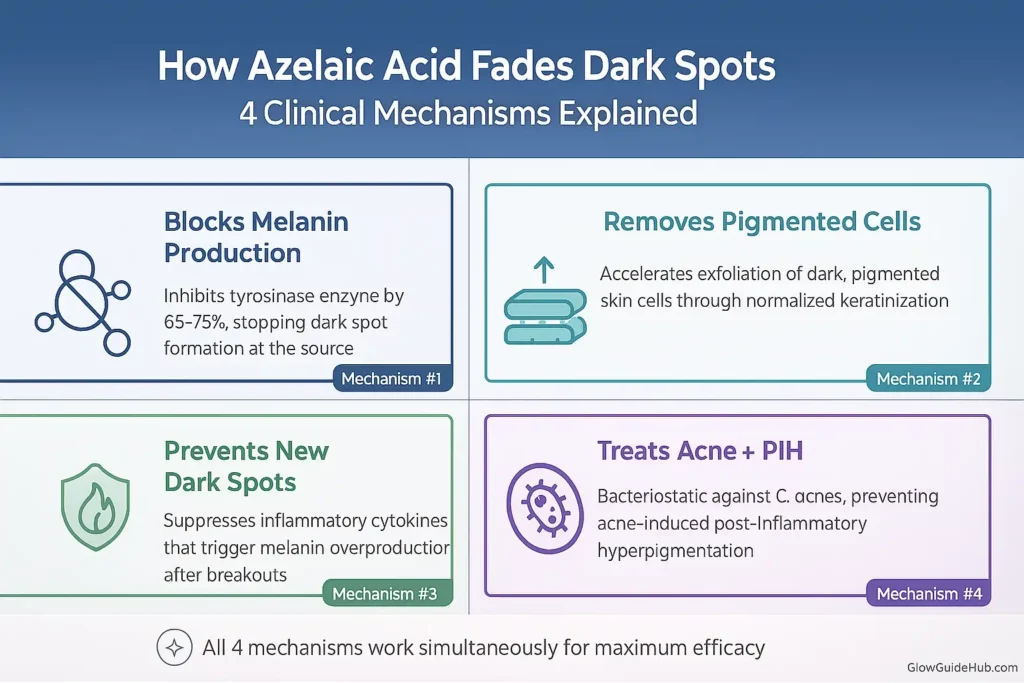
Azelaic acid treats hyperpigmentation through four distinct, clinically validated mechanisms:
(1) Competitive tyrosinase inhibition that reduces melanin synthesis by 65-75%,
(2) Keratolytic action that accelerates pigmented cell removal through normalized keratinization,
(3) Anti-inflammatory effects that suppress cytokine-mediated melanogenesis, and
(4) Bacteriostatic activity against Cutibacterium acnes that prevents inflammation-induced PIH.
Let’s dig deeper.
Mechanism #1: Tyrosinase Inhibition (Blocks Melanin Production)
What happens: Azelaic acid competitively inhibits tyrosinase—the key enzyme your skin cells use to produce melanin (the pigment that creates dark spots).
The science: Melanin production follows this pathway:
Tyrosine (amino acid) → DOPA → DOPAquinone → Melanin
↑ Tyrosinase enzyme catalyzes this.
Azelaic acid blocks tyrosinase activity, stopping melanin production at the source.
Why this matters: Research demonstrates that azelaic acid significantly reduces tyrosinase activity in hyperactive melanocytes—the cells responsible for dark spots and PIH. This targeted action means it fades hyperpigmentation effectively while preserving your skin’s normal tone, making it safer than many other brightening agents.
Mechanism #2: Keratolytic Action (Removes Pigmented Cells Faster)
What happens: Azelaic acid gently accelerates the shedding of pigmented dead skin cells from the surface.
How it works:
- Reduces keratin production in skin cells
- Loosens bonds between dead cells
- Speeds up natural exfoliation
- Brings deeper pigmented cells to the surface faster
Why this matters: This mechanism is gentler than AHAs or BHAs because it works at your skin’s natural pH (4.0-5.5) without compromising your skin barrier.
A 16-week study showed that 15% azelaic acid gel reduced post-inflammatory hyperpigmentation through combined tyrosinase inhibition and keratolytic action.
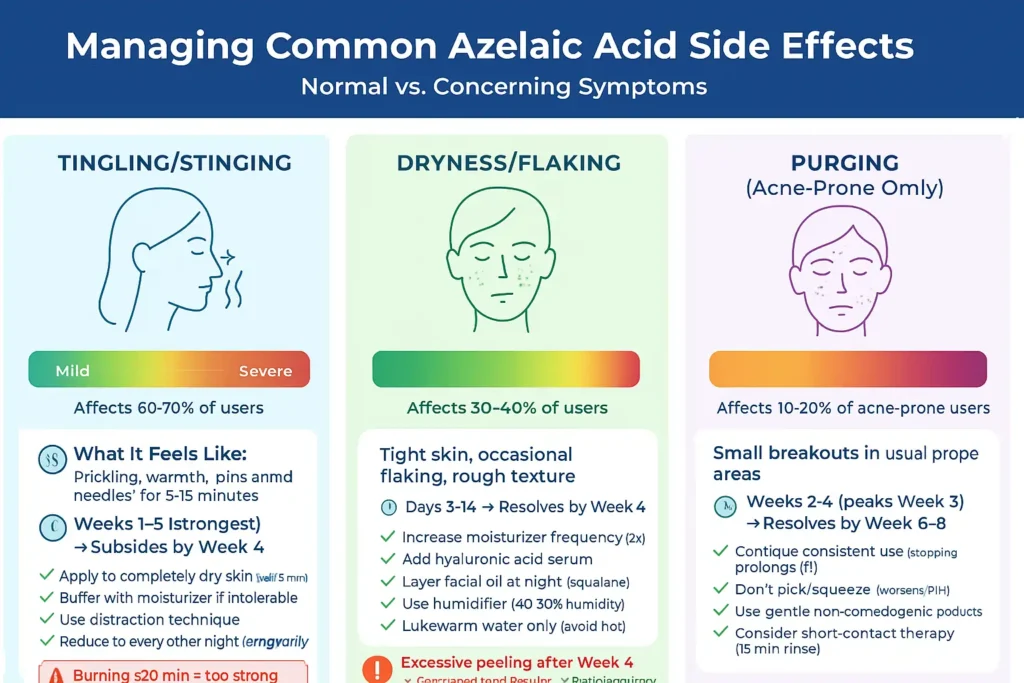
Practical impact: You’ll see slight flaking in weeks 2-4. That’s not irritation—it’s pigmented cells shedding. Don’t pick at them; let the process happen naturally.
Mechanism #3: Anti-Inflammatory Properties (Prevents New Dark Spots)
What happens: Azelaic acid suppresses inflammatory mediators that trigger excess melanin production.
The cascade: Inflammation is a major hyperpigmentation trigger because:
Inflammation → Releases cytokines (IL-1β, IL-6, TNF-α)
↓
Cytokines stimulate melanocytes → Excess melanin production.
↓
Result: Post-inflammatory hyperpigmentation (PIH)
Azelaic acid inhibits reactive oxygen species (ROS) production and downregulates proinflammatory compounds, reducing oxidative tissue damage at inflammation sites.
Real-world impact: This is why azelaic acid is perfect for acne-prone skin with PIH:
- ✓ Treats active acne (antibacterial effect)
- ✓ Calms inflammation (prevents PIH formation)
- ✓ Fades existing PIH (mechanisms 1 & 2)
Three problems solved with one ingredient.
Critical for darker skin tones: Fitzpatrick skin types IV-VI are at higher risk for PIH because inflammation triggers more aggressive melanin responses. Azelaic acid’s anti-inflammatory properties prevent the hyperpigmentation cascade from starting.
Mechanism #4: Antibacterial Effects (Stops Acne-Related PIH)
What happens: Azelaic acid exhibits bacteriostatic activity against Cutibacterium acnes (formerly Propionibacterium acnes) and other bacteria.
Why this matters for hyperpigmentation: The connection isn’t obvious at first, but here’s the cascade:
Acne bacteria → Inflammatory breakout
↓
Inflammation → PIH (mechanism #3 explains this)
By preventing breakouts, azelaic acid prevents the PIH that those breakouts would cause.
A clinical trial found that 20% azelaic acid gel reduced acne severity by 65.2% over 6 weeks—proving more than three times as effective as a placebo in treating mild-to-moderate acne.
The dual benefit: Most hyperpigmentation treatments are passive (only fade existing spots). Azelaic acid is active + preventive:
- ✓ Fades existing PIH
- ✓ Prevents new PIH from forming
This is why consistent long-term use yields dramatically better results than spot treatment.
Why These 4 Mechanisms Matter Together
Most brightening ingredients work through ONE mechanism:
- Vitamin C = antioxidant protection
- Hydroquinone = tyrosinase inhibition only
- Niacinamide = melanin transfer inhibition
- Kojic acid = tyrosinase inhibition only
Azelaic acid works through FOUR simultaneous mechanisms:
- Blocks melanin production (tyrosinase inhibition)
- Removes existing pigmentation (keratolytic)
- Prevents inflammation-triggered pigmentation (anti-inflammatory)
- Prevents acne-related PIH (antibacterial)
Result: More comprehensive, longer-lasting results—but they take 8-12 weeks to fully manifest because all four mechanisms need time to work synergistically.
What Types of Hyperpigmentation Does Azelaic Acid Treat?
Not all dark spots respond equally to azelaic acid. Here’s exactly when to use it—and when to look elsewhere.
Post-Inflammatory Hyperpigmentation (PIH)
Post-inflammatory hyperpigmentation (PIH) is a common dermatological condition characterized by flat, discolored patches that develop following skin inflammation or injury. This occurs when trauma triggers melanocytes—the pigment-producing cells—to overproduce melanin as part of the skin’s natural healing response.
PIH appears as brown, tan, or dark marks that persist long after the initial inflammation has resolved, affecting all skin types but manifesting more prominently in individuals with darker complexions due to higher baseline melanin activity.
Post-inflammatory hyperpigmentation is the dark spots left behind after:
- Acne breakouts (most common)
- Cuts, burns, or injuries
- Eczema or psoriasis flares
- Insect bites or allergic reactions
Why azelaic acid excels for PIH:
Because it:
- Treats active acne while fading old PIH
- Prevents NEW PIH from forming (anti-inflammatory)
- Safe for inflamed, healing skin
- Works across all Fitzpatrick skin types (I-VI)
Expected timeline:
- Weeks 1-4: No visible change (be patient!)
- Weeks 6-8: 30-40% lighter
- Weeks 12-16: 70-80% improvement
Realistic expectation: Most PIH will fade 70-90%. Complete erasure is rare for very dark or old PIH.
Melasma: GOOD (With Realistic Expectations)
What is melasma?
Melasma is a chronic hyperpigmentation disorder characterized by symmetrical brown or gray-brown patches on sun-exposed facial areas. Triggered by hormonal fluctuations, UV exposure, and genetic factors, it predominantly affects women of reproductive age with darker skin types, making it a notoriously persistent pigmentary condition requiring comprehensive photoprotection and dermatological treatment.
Hormonal hyperpigmentation appearing as:
- Symmetrical patches on the cheeks, forehead, and upper lip
- Triggered by pregnancy, birth control, and menopause
- Worsened by sun, heat, and hormones
Why azelaic acid works for melasma:
- ✓ FDA-approved treatment for melasma
- ✓ Safer than hydroquinone for long-term management (no ochronosis risk)
- ✓ Doesn’t cause rebound darkening when stopped
- ✓ Effective in darker skin tones (Fitzpatrick IV-VI)
A randomized controlled trial showed 20% azelaic acid delivered equal efficacy to 4% hydroquinone at 24 weeks, with significantly greater patient satisfaction and lower side effect rates.
The truth about melasma:
- Azelaic acid alone: 40-60% improvement
- Combination therapy (gold standard): 70-80% improvement
- Maintenance required: Melasma returns in 90% of cases without ongoing treatment
Best protocol for melasma:
Solo Treatment:
- 15-20% azelaic acid (prescription strength required)
- Apply nightly for 4-6 months
- SPF 50+ reapplied every 2 hours during the day
- Expect 50-60% lightening
Combination Protocol (Dermatologist-Recommended):
- Morning: Niacinamide 5% serum + Vitamin C 15% + SPF 50+
- Evening: Azelaic acid 15-20%
- 2-3x weekly: Tretinoin 0.025-0.05% (alternate nights with azelaic acid)
- Consider: Oral tranexamic acid (prescription, if appropriate candidate)
Expected timeline:
- Weeks 1-8: Minimal visible change (frustrating but normal—don’t quit!)
- Weeks 10-16: 20-30% lightening begins
- Months 4-6: Maximum results (60-70% improvement)
- Ongoing: Continue 3-5x weekly FOREVER (maintenance therapy)
⚠️ Critical caveat: Melasma treatment NEVER ends. If you stop completely, it returns within months. Think of azelaic acid as long-term management, not a cure.
Sun Spots (Solar Lentigines): MODERATE
What are sunspots?
Sunspots, clinically known as solar lentigines, are benign hyperpigmented lesions resulting from years of cumulative ultraviolet radiation exposure. These flat, well-demarcated brown macules develop when chronic sun damage triggers localized melanocyte hyperactivity and uneven melanin distribution.
Predominantly appearing in individuals over 40, sunspots represent visible markers of photodamage and require consistent sun protection to prevent further development.
- Flat brown spots from cumulative UV damage
- Also called age spots, liver spots
- Appear on face, hands, shoulders, décolletage
- More common in people 40+
Azelaic acid effectiveness:
- ✓ Gradual fading over 3-6 months
- ✓ Prevents new spots while treating existing ones
- ✓ Safe for large treatment areas (unlike lasers)
- ✗ Slower than professional treatments (IPL, laser, chemical peels)
- ✗ May not fully eliminate very dark or large spots
When to choose azelaic acid over laser:
- Budget constraints (topical = $8-60 vs laser = $500-2,000 per session)
- Mild to moderate sun damage
- Prefer gradual, natural-looking results
- High skin sensitivity or reactivity
- Maintenance after professional treatment
Expected timeline:
- Months 1-2: Minimal change (pigment is deeper in dermis)
- Months 3-4: 40-60% fading
- Months 5-6: Maximum results (60-80% lighter)
Realistic outcome: Spots will lighten significantly but rarely disappear completely. Think “75% lighter,” not “100% gone.”
Dark Circles: LIMITED EFFECTIVENESS
The problem: Dark circles have THREE different causes—azelaic acid only helps ONE type.
Type 1: Pigmented Dark Circles (Brown/Tan)
- Cause: Excess melanin deposition in the under-eye area
- Azelaic acid effectiveness: May help moderately
- Timeline: 4-6 months of consistent use
- Safety concern: Standard concentrations (15-20%) are too harsh for the delicate eye area
- Recommendation: Use 10% formulations only, patch test first, apply sparingly
For targeted under-eye product recommendations, explore our full guide.
Type 2: Vascular Dark Circles (Blue/Purple)
- Cause: Visible blood vessels through thin skin
- Azelaic acid effectiveness: Won’t help (not a pigmentation issue)
- Better options: Caffeine serums, vitamin K, retinaldehyde, laser treatments
Type 3: Structural Dark Circles (Shadowing)
- Cause: Under-eye hollows, loss of volume, orbital fat pad descent
- Azelaic acid effectiveness: Won’t help (structural problem)
- Better options: Hyaluronic acid fillers, fat grafting, lower blepharoplasty
My recommendation:
Skip azelaic acid for dark circles. Better, more targeted alternatives exist:
-
Caffeine + peptide eye serum (reduces puffiness, strengthens capillaries)
-
Vitamin K oxide eye cream (addresses vascular component)
-
Retinaldehyde 0.05% eye product (gentle retinoid for pigmentation + collagen support)
For a list of the top dermatologist-approved options, check out my detailed guide here:
What Azelaic Acid CAN’T Treat (Don’t Waste Your Time)
Freckles: DO NOT TREAT
- Freckles are genetic (ephelides), not a “skin problem.”
- Attempting removal can damage skin and cause inflammation-induced hyperpigmentation.
- Embrace them—they’re beautiful and natural
- If temporary fading is desired for events, Vitamin C is a gentler option
Birthmarks (Congenital Melanocytic Nevi): DO NOT TREAT
- Deep pigment deposits are present from birth
- Cannot be treated with topical products
- Require a dermatologist evaluation
- Options if concerned: Laser, surgical removal (only if medically necessary)
Important warning: Never attempt to “bleach” freckles or birthmarks at home. This causes chronic irritation, uneven skin tone, potential permanent damage, and paradoxical post-inflammatory hyperpigmentation.
Actinic Keratosis & Suspicious Lesions: SEE DERMATOLOGIST
If you have dark spots that:
- ✗ Are raised, scaly, or crusty
- ✗ Have irregular or changing borders
- ✗ Change in size, shape, or color over time
- ✗ Bleed, crust over, or don’t heal
- ✗ Appear suddenly after age 40
DO NOT self-treat with azelaic acid. These require professional evaluation to rule out:
- Actinic keratosis (precancerous lesions)
- Seborrheic keratosis (benign but mimics melanoma)
- Lentigo maligna (melanoma in situ)
- Basal cell carcinoma, squamous cell carcinoma
Critical rule: When in doubt, get it checked out. Hyperpigmentation treatment can wait—skin cancer cannot.
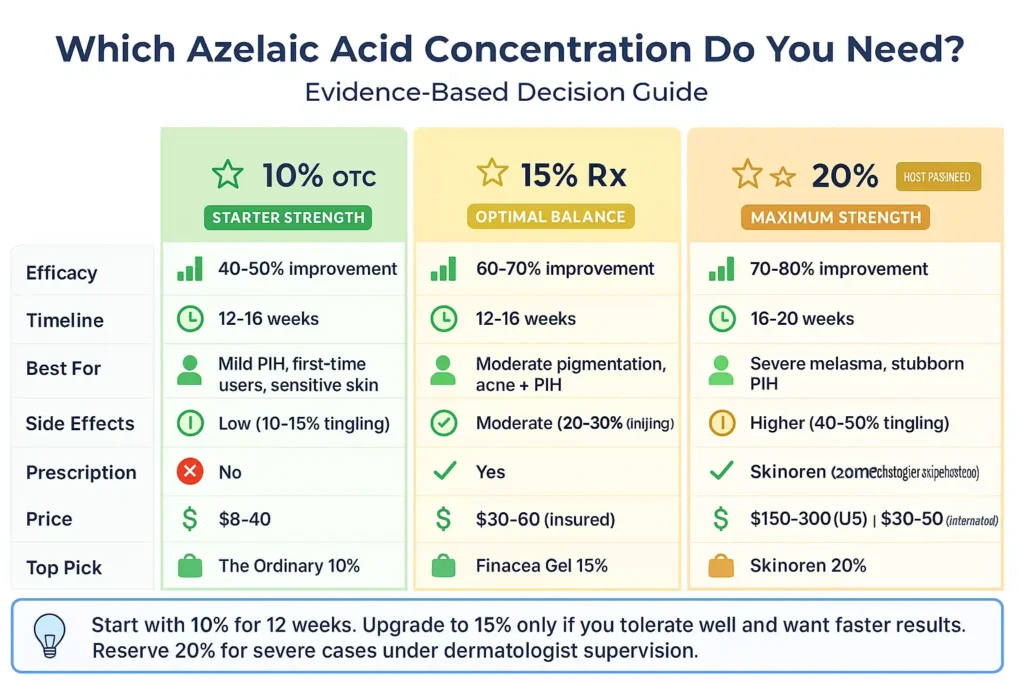
Which Concentration of Azelaic Acid Do You Need? (10% vs 15% vs 20%)
The honest answer: Most people should start with 10%—not because higher concentrations don’t work, but because consistency matters more than concentration.
Starting too strong causes irritation → inconsistent use → worse results than consistent 10% use.
10% Azelaic Acid (Over-the-Counter)
Efficacy: 40-50% pigmentation improvement over 12-16 weeks
Best for:
- First-time azelaic acid users
- Sensitive or reactive skin
- Mild post-inflammatory hyperpigmentation (PIH)
- Maintenance after clearing with a higher concentration
- Testing tolerance before prescription commitment
Pros:
- ✓ No prescription needed (buy online or in-store)
- ✓ Lower cost ($8-40)
- ✓ Lower irritation risk (10-15% of users experience tingling)
- ✓ Widely available (Ulta, Sephora, Amazon, brand websites)
- ✓ Can be used long-term without medical supervision
Cons:
- ✗ Slower results than prescription strength
- ✗ May plateau at 50% improvement (insufficient for severe cases)
- ✗ Requires an upgrade for stubborn pigmentation
My professional take: 10% is NOT “too weak.” Clinical studies demonstrate meaningful results with azelaic acid, though improvements occur gradually. Research in Clinical Therapeutics (1998) showed visible improvements at 8-12 weeks, continuing through 24 weeks¹. A study in the International Journal of Dermatology (1991) confirmed comparable efficacy to hydroquinone after 8-12 weeks². Start with 10% and if well-tolerated with visible improvement, consider upgrading to 15-20% prescription strength for accelerated results.
15% Azelaic Acid (Prescription)
Efficacy: 60-70% pigmentation improvement over 12-16 weeks
Best for:
- Moderate pigmentation unresponsive to 10%
- Combination acne + pigmentation
- Rosacea with hyperpigmentation
- Those who tolerated 10% but need better results
Pros:
- ✓ Clinically proven optimal balance (efficacy vs irritation)
- ✓ Most prescribed concentration by dermatologists
- ✓ Gel formulation available (Finacea—best for oily skin)
- ✓ FDA-approved for acne, rosacea, and melasma
Cons:
- ✗ Requires a dermatologist visit and prescription
- ✗ Higher cost ($30-60 with insurance, $200-300 without)
- ✗ Moderate irritation risk (20-30% experience initial tingling)
My professional recommendation: 15% is the “sweet spot” for most moderate-to-severe hyperpigmentation cases. If 10% gave you 40% improvement, but you want more, 15% will likely get you to 70% without the irritation risk of 20%.
How to get it:
- Schedule a dermatologist appointment (virtual or in-person—many insurances cover teledermatology)
- Discuss hyperpigmentation concerns and show before photos
- Request Finacea or generic azelaic acid 15% if appropriate
- Many insurance plans require prior authorization
20% Azelaic Acid (Prescription)
Efficacy: 70-80% pigmentation improvement over 16-20 weeks
Best for:
- Severe, stubborn melasma resistant to lower concentrations
- Treatment-resistant pigmentation that failed 10-15%
- Darker skin tones (Fitzpatrick V-VI) with significant PIH
- Under dermatologist supervision ONLY
Pros:
- ✓ Highest concentration available
- ✓ Maximum efficacy for severe cases
- ✓ Cream formulation (more hydrating than gel)
Cons:
- ✗ Requires prescription
- ✗ Expensive (Azelex in the US: $150-250 without insurance; Skinoren internationally: $30-50)
- ✗ Higher irritation potential (40-50% experience initial tingling/stinging)
- ✗ Cream texture may clog pores on very oily skin
Critical reality check: 20% does NOT equal “33% better results than 15%.” The relationship between concentration and efficacy is NOT linear.
Studies show:
- 10% → 15%: Significant efficacy increase
- 15% → 20%: Modest efficacy increase, higher irritation risk
My honest assessment: 20% is often overprescribed. Many patients would achieve the same results with 15% if they:
- Used it consistently for the full 16-20 weeks
- Applied proper sun protection (SPF 50+, reapplied every 2 hours)
- Combined strategically with niacinamide or tretinoin
Reserve 20% for truly stubborn cases that failed 15% after 20+ weeks of perfect compliance.
Decision Tree: Which Concentration Should You Start With?
Scenario 1: Mild PIH (Light Brown, Less Than 6 Months Old)
→ Start with 10% OTC
→ Reassess at 12 weeks
→ Upgrade to 15% only if plateaued, but want more improvement
Scenario 2: Moderate PIH or Early Melasma
→ Start with 10% OTC for 4-8 weeks (test tolerance)
→ Upgrade to 15% prescription if tolerated well and want faster results
→ OR continue 10% if seeing steady improvement (don’t fix what’s not broken)
Scenario 3: Severe Melasma or Very Dark, Stubborn PIH
→ See a dermatologist immediately
→ Likely start 15% with combination therapy (+ tretinoin, niacinamide, oral tranexamic acid)
→ Upgrade to 20% only if 15% fails after 20-24 weeks
Scenario 4: Sensitive/Reactive Skin
→ Always start 10%
→ Consider staying at 10% long-term even if results are slower
→ Irritation from 15-20% will worsen pigmentation (counterproductive)
Scenario 5: First-Time Active Ingredient User
→ 10% OTC for 12-16 weeks minimum
→ Build skin tolerance before considering stronger actives
→ Learn your skin’s response patterns
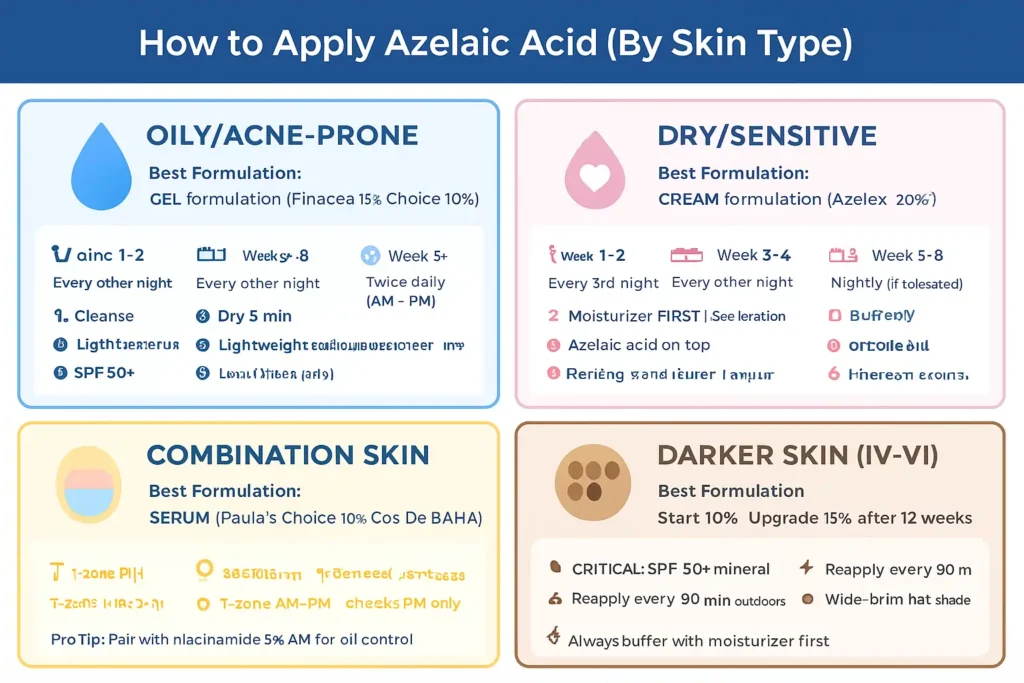
How to Use Azelaic Acid: Step-by-Step Application Protocol
The difference between success and failure often comes down to HOW you apply azelaic acid, not just which concentration you choose.
Basic Application Protocol (All Skin Types)
Step 1: Cleanse
- Use a gentle, non-stripping cleanser (avoid sulfates)
- Pat skin dry with a clean towel (don’t rub)
- Tip: Double cleanse at night if wearing sunscreen/makeup
Step 2: Wait 5 Minutes CRITICAL STEP
- Skin must be completely dry before applying azelaic acid
- Applying to damp skin increases penetration and the tingling sensation
- Use this time to brush teeth, prep other products, etc.
Step 3: Apply Azelaic Acid
- Amount: Pea-sized amount for entire face (less is more)
- Technique: Dot on forehead, cheeks, chin, nose
- Spread in a thin, even layer using gentle patting motions
- Avoid the eye area (stay 1cm away from the orbital bone)
Step 4: Wait 10 Minutes (Optional but Recommended)
- Allows full absorption before the next layer
- Reduces the risk of pilling with subsequent products
- Use this time for other skincare steps (neck cream, hand cream, etc.)
Step 5: Moisturize
- Apply your regular moisturizer
- Don’t skip this step (maintains barrier function)
- Choose a formula based on skin type (gel for oily, cream for dry)
Step 6: SPF (Morning Only)
- SPF 50+ broad-spectrum mineral or chemical sunscreen
- Apply 1/4 teaspoon to the face (most people use 1/4 of this amount)
- Reapply every 2 hours if outdoors or near windows
Application Protocols by Skin Type
For Oily/Acne-Prone Skin
Best formulation: Gel (Finacea 15% gel, Paula’s Choice 10% Booster)
Why: Lightweight, matte finish, absorbs quickly, won’t clog pores
Introduction Schedule:
- Weeks 1-2: Apply every other night only
- Weeks 3-4: Increase to nightly application
- Week 5+: Add morning application if tolerated
AM Routine:
📋 Medical Disclaimer
For Educational Purposes Only: This article is written by Kousar Subhan, a Medical Writer and Researcher, and is intended for informational and educational purposes only. The content provided is based on scientific research, peer-reviewed studies, and dermatological literature available as of December 2025.
Not Medical Advice: The information in this article does not constitute medical advice, diagnosis, or treatment recommendations. It should not be used as a substitute for professional medical consultation, diagnosis, or treatment from a board-certified dermatologist or qualified healthcare provider.
Individual Results May Vary: Skin conditions, including hyperpigmentation, melasma, and UV-induced pigmentation, vary significantly between individuals based on genetics, skin type, hormonal factors, and environmental exposure.
Consult Your Healthcare Provider: Before starting any new skincare regimen, especially if you are pregnant, breastfeeding, have diagnosed skin conditions, are taking medications, have sensitive skin, or are undergoing dermatological treatments.
Product Safety: Always perform a patch test before using new skincare products. Discontinue use and consult a healthcare professional if you experience irritation or adverse reactions.
🛍️ Affiliate Disclosure
Amazon Associates Program: Glow Guide Hub participates in the Amazon Services LLC Associates Program. When you purchase through our Amazon affiliate links, we may earn a small commission at no extra cost to you.
Editorial Independence: Our affiliate relationships do not influence our content or recommendations. We only recommend products based on scientific research, clinical evidence, and genuine quality assessment.
Supporting Our Mission: Your purchases through affiliate links help us maintain this free, evidence-based educational resource. Thank you for your trust!