How Stress Affects Pre-Existing Skin Conditions: Breaking the Cortisol-Skin Connection in 2025
 Did you know that chronic stress can lead to inflammation, which not only prevents acne from healing but can also trigger flare-ups of skin conditions such as rosacea, eczema, or psoriasis?
Did you know that chronic stress can lead to inflammation, which not only prevents acne from healing but can also trigger flare-ups of skin conditions such as rosacea, eczema, or psoriasis?
If you’re battling stubborn skin conditions that seem to worsen during challenging times, you’re not alone—and honestly, this connection still surprises many of my patients even today.
Drawing on my 18 years of experience in medicine and specialized training in Cosmetic Science, I’ve witnessed firsthand how stress can transform manageable skin conditions into overwhelming challenges.
Just last week, a patient told me her psoriasis “knew” when quarterly reports were due at work. She wasn’t imagining it. The connection between our emotional state and skin health runs deeper than most realize—and understanding this link is your first step toward healthier, calmer skin.
When life becomes overwhelming, your skin is often the first casualty. But here’s the empowering truth: by understanding how stress hormones affect your existing skin conditions, you can break this vicious cycle and reclaim control over your skin’s health.
And no, it’s not about eliminating stress (because let’s be real, who can do that?). It’s about working smarter with your body’s natural responses.
The Science Behind Stress-Skin Connection: Understanding Your Body’s Response
How Cortisol Damages Your Skin Barrier Function
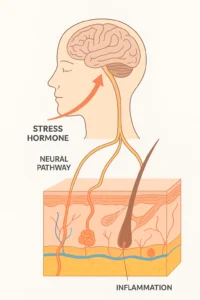
Let me paint you a picture of what happens inside your body during that morning traffic jam when you’re already running late. Your hypothalamic-pituitary-adrenal (HPA) axis—think of it as your body’s stress command center—kicks into overdrive. Cortisol floods your system like an unwanted house guest who won’t leave.
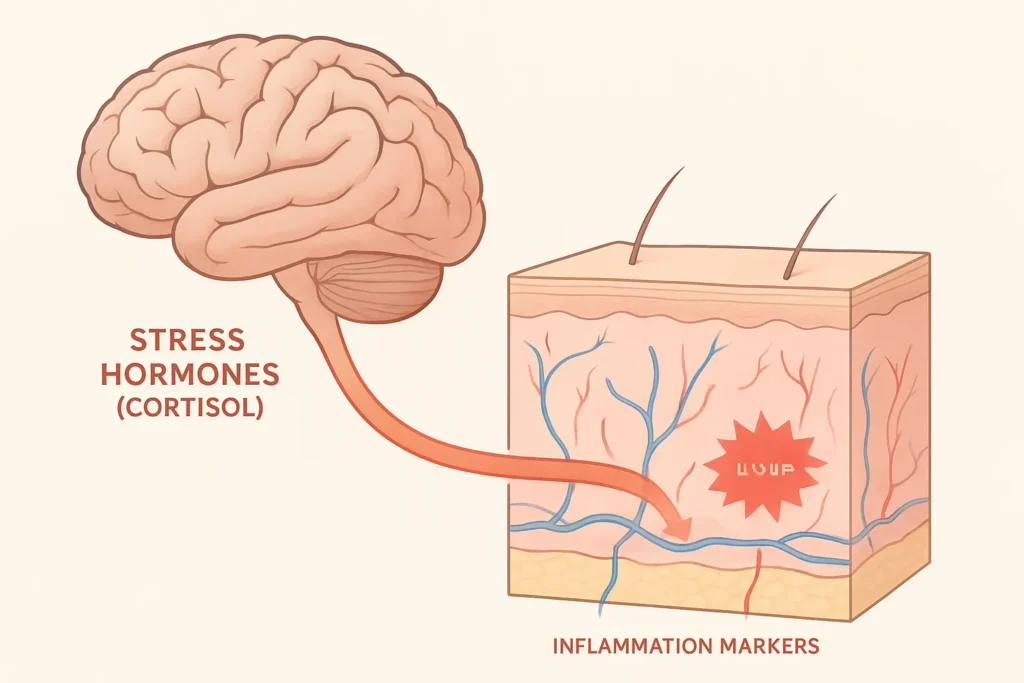
Here’s where it gets interesting. That cortisol doesn’t just make you feel weird; it literally compromises your skin barrier function. According to research from ScienceDirect (2023), stress triggers the release of pro-inflammatory cytokines that essentially tell your skin cells to panic. Your skin barrier, which is usually a fortress that keeps moisture in and irritants out, starts developing microscopic cracks.
Picture your skin barrier like a brick wall. Under normal conditions, the “mortar” between cells stays strong. But cortisol? It’s like acid rain on that mortar, slowly weakening the bonds. This explains why stressed skin feels dry, tight, and somehow more reactive to everything—even products you’ve used for years.
The cascade doesn’t stop there. Impaired wound healing becomes another casualty of chronic stress. Those minor blemishes that usually disappear in days? They linger for weeks. Why? Because cortisol suppresses your immune system’s repair crew, leaving damage unaddressed longer than necessary.
Neuroendocrine-Immune Interactions in Stressed Skin
Now, you might wonder how a deadline at work translates to angry red patches on your face. The answer lies in the fascinating (and frustrating) neuroendocrine-immune interaction. Your nervous system, hormone system, and immune system aren’t separate entities—they’re more like gossipy neighbors constantly talking over the fence.
When psychological stress hits, your brain sends distress signals through nerve pathways directly to your skin. These signals trigger mast cells—think of them as your skin’s alarm system—to release histamine and other inflammatory mediators. It’s basically your skin overreacting to a threat that isn’t physically there.
Research has consistently shown that stressed individuals with skin conditions exhibit elevated inflammatory markers. We’re talking about increased interleukin-6, tumor necrosis factor-alpha, and other substances with intimidating names that essentially mean “inflammation party in progress.” Your skin becomes a battlefield where your own immune system is both soldier and enemy.
The Vicious Cycle: How Skin Flares Create More Stress
And here’s the kicker—the relationship isn’t one-way. Your stressed-out skin stresses you out more, creating what dermatologists call a bidirectional relationship. You stress about a presentation, your eczema flares, you worry about the eczema, it gets worse. Rinse and repeat.
I recall a patient who canceled three appointments because her rosacea flared up during a particularly stressful month. The emotional toll of visible skin conditions can’t be understated.
Studies show that people with chronic skin conditions report quality of life impacts similar to those with heart disease or diabetes. Yet somehow, we still treat skin issues as “just cosmetic.”
The psychological impact creates its own stress response, perpetuating the cycle. Stress makes it harder for your skin to recover from damage because your body prioritizes immediate survival (even from imaginary tigers) over skin repair. Your healing resources get diverted, leaving your skin in a constant state of catch-up.
Major Skin Conditions Triggered and Worsened by Stress
Psoriasis: When Stress Triggers Immune System Overreaction
Psoriasis patients often know exactly when stress will trigger a flare—it’s almost like clockwork. According to dermatologists at the Cleveland Clinic, emotional stress ranks among the top triggers for psoriasis flare-ups, right alongside infections and weather changes.
During stressful periods, your immune system goes haywire, accelerating skin cell production from a regular 28-day cycle to just 3-4 days. These cells accumulate faster than your body can shed them, forming the characteristic silvery plaques. It’s like your skin is building a protective armor against a threat that exists only in your mind.
Managing stress-induced psoriasis isn’t just about slathering on topical steroids. One of my patients found that scheduling “worry time”—15 minutes daily to stress about things actively—paradoxically reduced her overall anxiety and flare frequency. Sometimes acknowledging stress rather than fighting it helps break its power over your skin.
Eczema and Atopic Dermatitis: Breaking the Itch-Stress Cycle
Eczema has a special relationship with stress—and not the good kind. The National Eczema Association (2025) emphasizes that stress plays a significant role in worsening eczema symptoms, particularly through cortisol’s disruption of the skin barrier.
For eczema sufferers, cortisol not only weakens the skin barrier but also amplifies the itch sensation. You know that maddening itch that gets worse the more you think about it?
That’s your nervous system and stress hormones working in tandem against you. The itch leads to scratching, which damages the skin, which in turn increases inflammation, which further exacerbates stress. It’s exhausting just thinking about it.
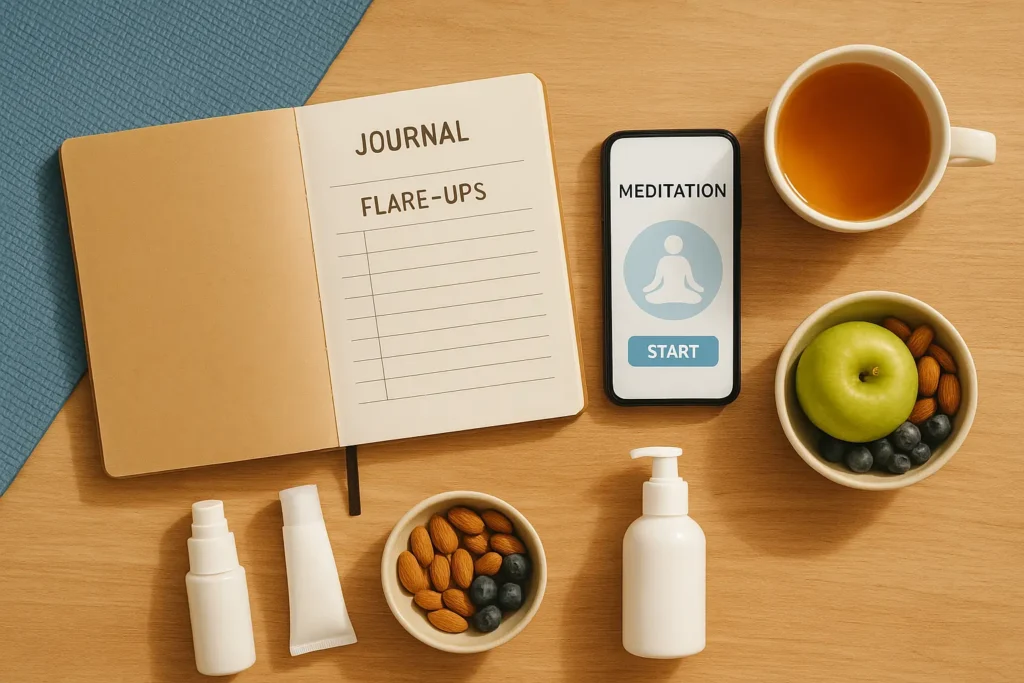
Personal stress triggers vary widely among eczema patients. Some react to work deadlines, others to relationship conflicts, and some to positive stress, such as planning a wedding. Identifying your unique triggers requires detective work—keeping a symptom diary alongside a stress log often reveals surprising patterns.
Rosacea: When Stress Shows on Your Face
Rosacea might be the most emotionally challenging stress-related skin condition because it’s so visible. Cortisol increases inflammation and dilates blood vessels, literally making stress show on your face. That facial flushing during an important meeting? It’s not just embarrassment—it’s cortisol exacerbating your rosacea symptoms.
The emotional triggers for rosacea patients create a ruthless cycle. Worrying about flushing often triggers flushing. Public speaking, first dates, and job interviews—situations where you most want clear skin become triggers themselves. It’s like your face has developed a terrible sense of timing.
Managing stress-induced rosacea requires both physical and mental strategies. Cool compresses help in the moment, but long-term management means addressing the underlying stress response. Some patients find that accepting potential flushing—literally saying “I might flush and that’s okay”—reduces the anxiety that triggers it.
Don’t skip sunscreen: Daily sun protection is non-negotiable for rosacea-prone skin. UV exposure worsens redness and inflammation, so dermatologists consistently recommend mineral-based sunscreens with zinc oxide to calm and protect the skin barrier.
Acne: The Cortisol-Sebum Connection
Adult acne deserves its own stress category. High cortisol levels don’t just cause inflammation; they stimulate sebaceous glands to produce more oil. Combine that with stress-weakened immunity, and you’ve got the perfect storm for breakouts. It’s why that giant zit appears right before important events—your skin has impeccable dramatic timing.
The cortisol-sebum connection explains why stress acne looks different from typical acne. These aren’t your teenage surface pimples; they’re deep, painful cystic breakouts that seem to emerge from nowhere. They’re tender, inflamed, and stubbornly resistant to typical acne treatments because the root cause isn’t bacterial—it’s hormonal.
Breaking the stress-breakout cycle requires patience. Unlike treating bacterial acne, addressing stress-induced acne means playing the long game. Quick fixes don’t exist because you’re dealing with systemic inflammation, not just clogged pores.
If you’re a teen interested in science-backed ways to calm breakouts, check out our dermatologist-approved guide here.
Recognizing Stress-Related Skin Flares: Early Warning Signs
Physical Symptoms to Watch For
Your skin often knows you’re stressed before you do. Those subtle signals—increased itching that starts as a tickle, burning sensations that come and go, or tingling that feels electric—these are your early warning system. Learning to recognize them can mean the difference between a minor irritation and a full-blown flare.
New lesions or patches appearing suddenly, especially in areas you don’t typically have issues, often signal stress involvement. Changes in skin texture—suddenly feeling sandpapery or unusually smooth—can indicate your barrier function is compromised. Even changes in how your skin feels to touch, becoming more sensitive or oddly numb, warrant attention.
Timing Patterns of Stress-Induced Flares
Here’s something fascinating: stress-related skin flares don’t always appear immediately. You might experience a delayed response—handling a crisis beautifully, only to break out in hives a week later when everything’s resolved. Your skin operates on its own timeline, processing stress days or even weeks after the trigger.
Keeping a symptom diary alongside life events reveals these patterns. Note, not just major stressors, but also positive stress—moves, promotions, even vacations can trigger flares. One patient discovered her eczema consistently flared exactly ten days after flying, correlating with her anticipatory travel stress rather than the trip itself.
Differentiating Stress Flares from Other Triggers
Not every flare-up stems from stress, and distinguishing its causes is crucial for effective treatment. Stress-induced reactions often exhibit characteristic features: they’re more widespread, appear in unusual patterns, and coincide with emotional events rather than environmental exposures.
Allergen-induced reactions typically appear quickly after exposure and follow consistent patterns. Stress flares? They’re sneakier, developing gradually and affecting areas that typically stay clear. Seasonal changes cause predictable patterns, while stress-related changes seem random until you connect the emotional dots.
Professional evaluation becomes crucial when patterns aren’t clear. A dermatologist can help differentiate between various triggers and may identify overlooked stressors that are affecting your skin.
Evidence-Based Stress Management Techniques for Clearer Skin
Mind-Body Interventions That Work
Let’s talk about what actually works, not just what sounds good in wellness magazines. Meditation isn’t just woo-woo nonsense—clinical studies consistently show measurable improvements in inflammatory markers after just eight weeks of practice. The University of Utah Health (2025) reports significant correlations between mindfulness practices and improved skin conditions.
Yoga combines physical movement with breathwork, targeting stress from multiple angles. But here’s the thing—you don’t need to become a yoga instructor. Even 10 minutes of simple stretches with focused breathing can lower cortisol levels.
Research in PubMed has shown that patients with psoriasis who practice yoga regularly experience significant reductions in Psoriasis Area and Severity Index (PASI) scores, along with improvements in skin hydration, reduced itching, and better sleep quality.
Exercise works, but with a caveat for individuals with skin conditions. Intense workouts can temporarily increase inflammation, potentially triggering flares. The sweet spot? Moderate exercise, such as walking, swimming, or cycling, for 30 minutes. Enough to release endorphins without overtaxing your system.
Journaling might seem old-school, but writing about stressors for 15 minutes daily has shown remarkable effects on skin healing. It’s like giving your brain a chance to process stress on paper instead of through your skin.
Lifestyle Modifications for Stress Reduction
Sleep optimization isn’t optional—it’s medicinal. Your cortisol levels naturally dip at night, allowing for skin repair. Disrupted sleep leads to sustained cortisol elevation, which sabotages overnight healing. Aim for 7-9 hours, but quality matters more than quantity. A consistent sleep schedule trains your cortisol rhythm.
Dietary changes that support stress resilience extend beyond avoiding sugar. Omega-3 fatty acids actively combat inflammation, while probiotics support the gut-skin axis. Yes, that’s a real thing—your gut bacteria influence skin inflammation through complex immune pathways.
Creating a skin-friendly daily routine means building in stress buffers. Morning routines that don’t involve rushing, lunch breaks that actually break from work, and evening wind-downs without screens. These aren’t luxuries; they’re preventive medicine for your skin.
Professional Therapeutic Approaches
Cognitive Behavioral Therapy (CBT) specifically for skin conditions exists, and it’s incredibly effective. Pfizer’s research highlights how CBT helps patients reframe thoughts about their skin, reducing both stress and symptom severity.
Biofeedback teaches you to control physiological responses you thought were automatic. Watching your stress levels on a monitor while learning to lower them feels like a superpower. Patients report not just clearer skin but feeling more in control generally.
Support groups offer something that medications can’t—understanding from people who genuinely understand. Online communities offer 24/7 support, while in-person groups provide deeper connections. The relief of saying “my skin is driving me crazy” to people who genuinely understand is therapeutically potent.
Integrative Treatment Strategies: Combining Stress Management with Medical Care

Working with Your Dermatologist During Stressful Periods
Communication with your dermatologist about life stressors isn’t oversharing—it’s crucial medical information. Knowing you’re going through a divorce or job change helps them adjust treatment proactively. Some dermatologists prescribe “stress doses” of medications during anticipated high-stress periods.
Preventive strategies for anticipated stress can make a huge difference. Planning a wedding? Starting preventive treatments three months prior can prevent the bride-to-be’s breakout. Going through exams? Adjusting skincare routines beforehand provides protective buffering.
Don’t wait for flares to communicate with providers. Regular check-ins during stressful periods enable minor adjustments, preventing major flare-ups. Think of it as preventive maintenance rather than emergency repairs.
Complementary Therapies for Stress-Related Skin Issues
Acupuncture’s effects on stress-related skin conditions surprised even the most skeptical. Studies have shown a reduction in inflammatory markers and an improvement in skin appearance following an acupuncture series. The mechanism isn’t fully understood, but the results speak volumes.
Aromatherapy sounds fluffy until you realize certain essential oils have measurable cortisol-lowering effects. Lavender isn’t just pleasant—it actively reduces stress hormones. But please, dilute properly—stressed skin is sensitive skin.
Massage therapy addresses stress through multiple pathways: physical tension release, improved circulation, and the psychological benefits of human touch. Regular massage isn’t an indulgence for stress-related skin conditions—it’s a therapeutic intervention.
Building a Personalized Stress-Skin Management Plan
Your stress trigger identification system needs to be personalized because generic advice fails. Maybe work stress doesn’t affect your skin, but family dynamics trigger immediate flares. Creating your unique trigger map takes time but provides invaluable insight.
Emergency action plans for flares should be written when calm, not created during crises. Include specific steps: medications to use, people to contact, activities to avoid. Having a plan reduces panic when flares occur, preventing stress escalation.
Long-term resilience building isn’t about eliminating stress—it’s about changing your relationship with it. This means consistent daily practices, not heroic efforts during flares.
Breaking the Cycle: Long-Term Solutions for Stress-Sensitive Skin
Developing Emotional Resilience
Building coping mechanisms for chronic conditions requires acknowledging the emotional toll. It’s okay to grieve the perfect skin you might never have. Acceptance doesn’t mean giving up—it means stopping the fight against reality that creates additional stress.
Acceptance and commitment therapy techniques teach living fully despite skin conditions. The goal isn’t loving your flares but accepting them as part of your experience without letting them define you.
Creating a support network specifically for skin health might feel excessive, but it’s essential. This includes understanding friends, knowledgeable healthcare providers, and possibly online communities. Isolation worsens both stress and skin conditions.
Preventive Measures for Future Flares
Stress inoculation training may sound intense, but it’s simply about practicing stress management when you’re calm. Like fire drills, you’re training responses for when real stress hits. Regular practice during calm periods makes techniques automatic during times of crisis.
Maintaining consistent skincare during calm periods may feel pointless when your skin looks good, but it’s actually building resilience reserves. Think of it as depositing into a skin health savings account you’ll need during stressful withdrawals.
Regular mental health check-ins, even when skin is clear, maintain emotional equilibrium. Therapy isn’t just for crisis—it’s preventive maintenance for your emotional and skin health.
Success Stories and Case Studies
Real patient experiences provide hope and practical insights. Sarah, a 34-year-old teacher, saw her psoriasis coverage reduce from 30% to 5% after implementing daily meditation and therapy. It took six months, but the results lasted.
Timeline expectations matter for maintaining hope. Most patients see initial improvements within 2-4 weeks of consistent stress management, with significant changes at 8-12 weeks. But remember—this isn’t a race. Sustainable improvement beats quick fixes.
Maintaining progress during challenging times requires flexibility and adaptability. Life happens—parents get sick, jobs change, relationships end. Having strategies for high-stress periods prevents complete reversals of progress.
Conclusion: Stress Affects Pre-Existing Skin Conditions
Living with a pre-existing skin condition doesn’t mean you’re destined to suffer through stress-related flares forever. Through my years in medicine and cosmetic science, I’ve seen remarkable transformations when patients understand and address the connection between stress and skin.
Remember, stress can negatively affect your skin by causing acne, dryness, wrinkles, rashes, and inflammation, but you’re not powerless against it. The tools I’ve shared—from understanding cortisol’s effects to implementing evidence-based stress management—aren’t just theories. They’re practical strategies that work.
Start small—pick one technique that resonates with you. Maybe it’s five minutes of morning meditation or keeping a stress-skin diary. Consistency matters more than perfection. Your skin didn’t develop stress sensitivity overnight, and healing happens gradually.
What matters most isn’t achieving stress-free living (impossible) or perfect skin (unrealistic). It’s finding your personal balance where stress becomes manageable and your skin becomes predictable. That’s not just achievable—it’s transformative. And honestly? You deserve skin that doesn’t hold you hostage to every stressful moment life throws your way.
FAQs: How Stress Affects Pre-Existing Skin Conditions
What Skin Conditions Are Triggered Or Worsened By Stress?
Stress can trigger or worsen eczema, psoriasis, acne, rosacea, hives, and seborrheic dermatitis. It also aggravates autoimmune skin conditions like vitiligo and alopecia areata by increasing inflammation and disrupting immune balance. Managing stress helps reduce flare frequency and intensity.
How Does Stress Impact Skin Conditions?
Chronic stress elevates cortisol, which weakens the skin barrier, slows healing, and triggers inflammation. This often causes flare-ups in eczema, psoriasis, and acne, creating a cycle where emotional stress and visible skin symptoms feed each other.
Is Skin Damage From Stress Reversible?
Yes. Most stress-related skin damage—such as dullness, dryness, and breakouts—can improve with stress reduction, adequate sleep, and barrier-repair skincare. Persistent conditions may need dermatologist-guided treatment and long-term stress management to fully restore healthy skin function.
How To Get Rid Of Stress-Related Spots?
Treat stress acne by balancing cortisol naturally—sleep, exercise, and mindfulness help regulate oil production. Use non-comedogenic skincare with niacinamide, salicylic acid, or zinc. Consistent stress management reduces new breakouts and promotes clearer skin.
What Vitamins Help Stressed Skin?
Key nutrients for stressed skin include Vitamin C (collagen repair), Vitamin E (antioxidant protection), B-complex vitamins (support barrier function), and Magnesium (reduces cortisol). A balanced diet plus hydration improves resilience and skin recovery under stress.
How Long Does It Take For Stress To Show On Your Skin?
Stress hormones affect skin within hours, but visible redness, acne, or eczema flares appear after 24–72 hours of continuous stress. Chronic stress leads to ongoing dullness and barrier damage if unmanaged.
What Are The First Signs That Stress Is Affecting My Skin?
Early warning signs include tightness, redness, dryness, itching, and increased sensitivity. You might notice your usual products start stinging or your skin looks dull—indicating rising inflammation and dehydration.
Can Stress Cause Permanent Damage To Skin Conditions?
Chronic stress rarely causes permanent damage, but prolonged inflammation can worsen scarring, pigmentation, and barrier weakness. Managing stress early prevents lasting texture or tone changes.
How Long Does It Take For The Body To Recover From Stress?
Skin usually improves within 2–4 weeks after consistent stress reduction. Severe flare-ups from psoriasis, eczema, or cystic acne may need 6–12 weeks of combined lifestyle and dermatological therapy for full recovery.
Disclaimer: GlowGuideHub participates in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for sites to earn advertising fees by advertising and linking to Amazon.com. As an Amazon Associate, I earn from qualifying purchases. If you click on an Amazon link on my site and make a purchase, I may earn a commission at no additional cost.
📋 Medical Disclaimer
For Educational Purposes Only: This article is written by Kousar Subhan, a Medical Writer and Researcher, and is intended for informational and educational purposes only. The content provided is based on scientific research, peer-reviewed studies, and dermatological literature available as of December 2025.
Not Medical Advice: The information in this article does not constitute medical advice, diagnosis, or treatment recommendations. It should not be used as a substitute for professional medical consultation, diagnosis, or treatment from a board-certified dermatologist or qualified healthcare provider.
Individual Results May Vary: Skin conditions, including hyperpigmentation, melasma, and UV-induced pigmentation, vary significantly between individuals based on genetics, skin type, hormonal factors, and environmental exposure.
Consult Your Healthcare Provider: Before starting any new skincare regimen, especially if you are pregnant, breastfeeding, have diagnosed skin conditions, are taking medications, have sensitive skin, or are undergoing dermatological treatments.
Product Safety: Always perform a patch test before using new skincare products. Discontinue use and consult a healthcare professional if you experience irritation or adverse reactions.

